Dysphagia and Swallowing
Published: 27 September 2022
Published: 27 September 2022
Dysphagia is a common condition seen in many long-term care clients, with chewing and swallowing problems affecting between 30 and 50% of Australian aged care residents (Aged Care Guide 2019).

Dysphagia is difficulty swallowing. This can include having problems with:
(Healthdirect 2020)
Dysphagia can make swallowing painful, and in some cases, impossible (Mayo Clinic 2021). People with dysphagia may experience gagging, coughing or choking when eating and drinking (SPA 2022).
Note: While dysphagia sounds similar to dysphasia, these two terms refer to separate conditions. While dysphagia is difficulty with swallowing, dysphasia (also known as aphasia) is difficulty with speaking. Even though these are two different conditions, they both commonly affect people who have had a neurological event such as a stroke, and are both treated by speech pathologists (Brouhard et al. 2022).
Dysphagia is not necessarily part of the normal ageing process (Health.vic 2015). However, it is not uncommon for older adults to experience presbyphagia - age-related changes to the swallowing mechanism (Thiyagalingam et al. 2021).
Presbyphagia can include:
(Thiyagalingam et al. 2021; Nestle Health Science 2018)
While presbyphagia can be a predisposing factor to dysphagia, an older adult’s swallow is not inherently an issue (Thiyagalingam et al. 2021; MSAC 2018). Instead, dysphagia is most commonly associated with underlying conditions that have a greater prevalence in older populations (Smithard et al. 2016) and interrupt the swallowing process, such as:
(Aged Care Guide 2019; Healthdirect 2020; Thiyagalingam et al. 2021)
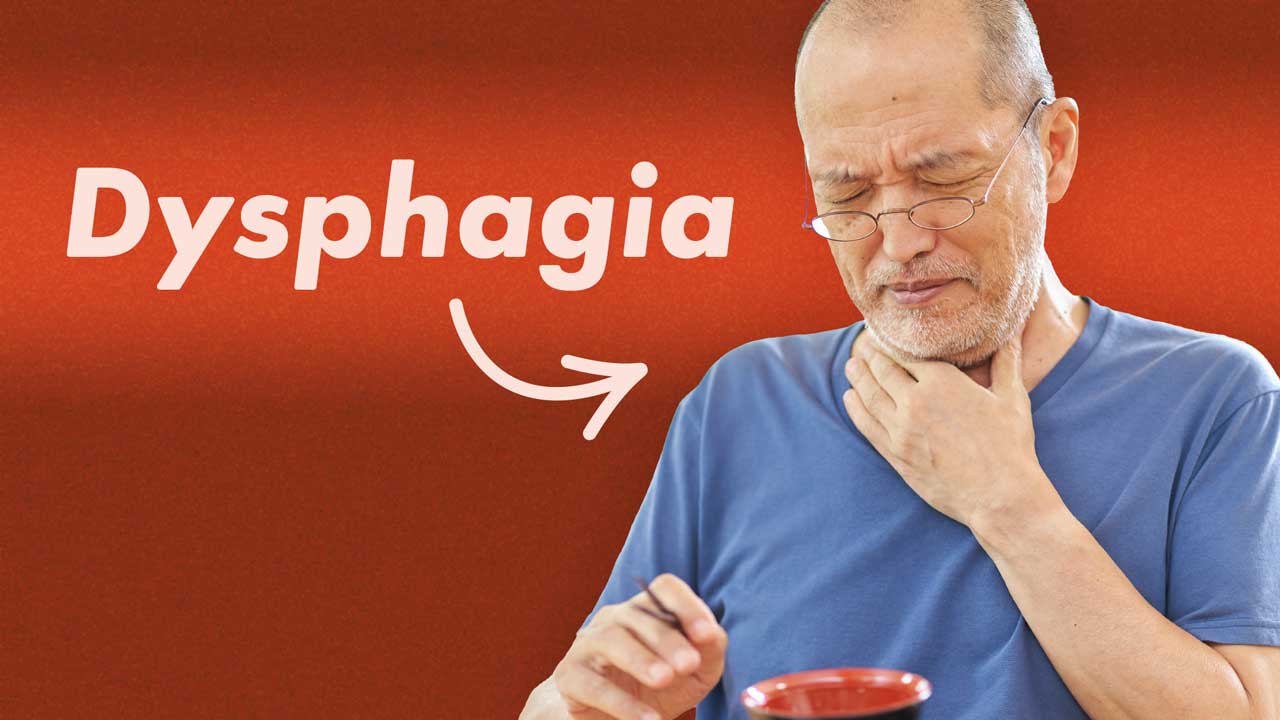
The swallow process is broken down into three stages: oral, pharyngeal and oesophageal. Dysphagia can affect just one of these phases of a combination of all three. Because of the nature of the swallow process, oral and pharyngeal dysphagia are often grouped together - this is known as oropharyngeal dysphagia.
Oropharyngeal dysphagia is difficulty moving food and fluids around the mouth, forming a bolus (the chewed up mass of food to be swallowed) and ‘initiating a swallow’. This type of dysphagia is commonly associated with stroke, dementia and Parkinson’s disease (Health.vic 2015; Nestle Health Science 2018).
Signs and symptoms of dysphagia can include:
(Mayo Clinic 2021; SPA 2019)
Clients displaying the above symptoms may require referral to a speech pathologist, who will assess and provide intervention for the swallowing difficulty. This may include recommending food texture and drink thickness modifications to manage the risk of eating and drinking, and teaching swallow rehabilitation exercises and safe swallowing strategies. Speech pathologists can also conduct videofluoroscopy (VFSS) and fiberoptic endoscopic evaluation of swallowing (FEES) to assess swallow safety. In severe cases, the client might require enteral feeding (SPA 2019).
Dysphagia can cause aspiration - where food, liquid or saliva tracks into or is inhaled into the lungs rather than being ingested into the stomach (Health.vic 2015).
This, in turn, can lead to aspiration pneumonia, an extremely serious and potentially fatal complication. Aspiration pneumonia is the most common cause of death in people with dysphagia (Health.vic 2015).
Factors that can increase the risk of developing aspiration pneumonia are:
(Langmore et al. 1998)
Dysphagia can also cause choking, which is the second most common cause of preventable death in aged care facilities (Aged Care Guide 2019).
Furthermore, people with dysphagia are at increased risk of developing malnutrition or dehydration if they cannot consume adequate amounts of food and fluid due to their condition (Healthdirect 2020).
Note: This Article is NOT an official IDDSI resource and is NOT meant to replace materials and resources on https://iddsi.org/. For the most current information and resources, see https://iddsi.org/.
.
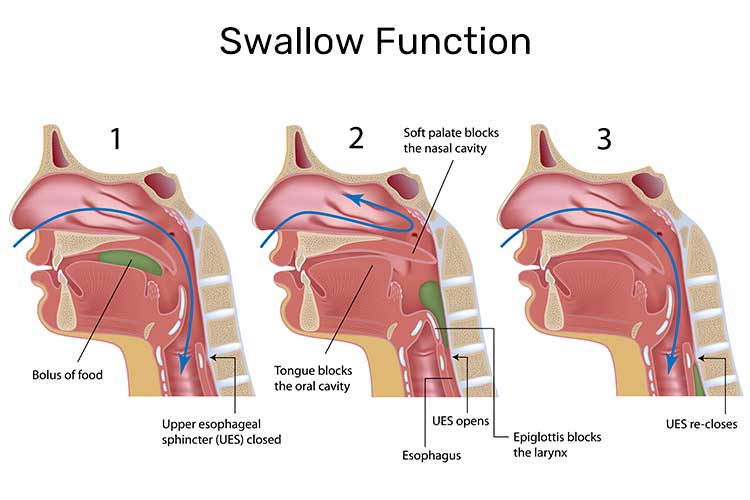
The International Dysphagia Diet Standardisation Initiative (IDDSI) is the global standard of texture modification for people with dysphagia, regardless of age or care setting (IDDSI 2020).
Depending on a client’s swallow test (usually performed by a speech pathologist), they will be prescribed a particular consistency of liquid to match their ability.
Liquid consistency can be anywhere from puree-thick, to runny and thin.
(IDDSI 2020)
Some of these fluids will come pre-prepared to the desired consistency, but others may need to have fluid thickener added to achieve the correct consistency for your client.
Like liquids, foods should be served at a manageable consistency as well, depending on the client’s ability to chew or swallow.
(IDDSI 2020)
Some people will be on normal consistency foods and can eat anything that they choose, while others may be at the stage of consuming slightly thickened liquids in addition to normal consistency food.

For all diet description information, please visit: https://www.iddsi.org/IDDSI/media/images/Complete_IDDSI_Framework_Final_31July2019.pdf
Dysphagia can make it slow, difficult and tiring to eat. This reduces the amount and variety of foods and drinks the person can consume, which in turn, can make it difficult to maintain adequate levels of nutrition and hydration (British Nutrition Foundation 2019).
While texture-modified foods and drinks are easier and safer for people with dysphagia to consume, they can cause unappealing changes to appearance, flavour and mouthfeel. Therefore, some clients may refuse or hesitate to consume them, which further increases the risk of malnutrition and dehydration (British Nutrition Foundation 2019).
Using moulds - for example, forming carrot puree into the shape of a carrot using a mould - may help make texture-modified food more palatable and easier to identify than a nondescript coloured blob. Another strategy to make texture-modified foods more appetising is to use flavoured foams and dusts (e.g. bacon dust) (Egan 2019).
People with dysphagia can often find it difficult to swallow tablets and capsules. Due to a lack of availability of other forms of medicine such as oral liquids, patches and suppositories, medication crushing is common in aged care facilities. However, altering the form of a solid medicine is a ‘significant source of medication error and harm to patients’ and can lead to adverse outcomes such as increased toxicity, reduced efficacy and instability of the medicine (Taylor & Glass 2018).
Therefore, medication frushing must only take place after referring to the medicine’s guidelines, references and/or product information (Taylor & Glass 2018).
Consider the following alternative options instead:
(Taylor & Glass 2018)
Good oral hygiene is especially important to maintain in older adults with dysphagia. This is because the mouth contains germs, pathogens and bacteria. If unclean saliva is aspirated, this can, in turn, increase the risk of developing serious aspiration pneumonia. Extra care needs to be taken to remove the build-up of food, drink and bacteria from the mouth (Hanrahan Health 2019).
(Loret 2015; Pines of Sarasota 2016; IDDSI 2019)
The following signs and symptoms are indicative of aspiration pneumonia and require immediate medical treatment:
(NHS 2021)
Question 1 of 3
Pureed food is numbered at which level of food thickness?
Peer reviewed by