Despite about 12% of aged care residents taking antimicrobials on any given day, only one-quarter of these clients are actually displaying signs of infection (DoHaAC 2023).
Antimicrobials is the broad term used to describe all medications that destroy or slow the growth of disease-causing pathogens (viruses, bacteria, parasites and fungi). Antibiotics are the specific type of antimicrobial used to treat bacterial infections (Australian Government 2022a).
This article will focus on the use of antibiotics in aged care.
Antibiotics and Aged Care
Aged care residents are often frail, have weak immune systems and live in close proximity to others, making them more susceptible to developing infections. This, in turn, correlates to increased antibiotic use in these facilities (Australian Government 2022b).
However, with the World Health Organisation declaring antimicrobial resistance (AMR) a major health concern, the prevalence of antibiotics in aged care poses a significant threat to a vulnerable population. In order to minimise the risk of antibiotic-resistant infections emerging and spreading in these environments, it is critical to prescribe and manage antibiotics appropriately (WHO 2021; Australian Government 2022b).
Using antibiotics appropriately means:
- Accurately assessing the client
- Confirming the client’s condition
- Prescribing the correct antibiotic
- Prescribing the correct dose
- Administering antibiotics through the correct route
- Administering antibiotics at the correct time
- Administering antibiotics for the correct duration of time
- Conducting timely reviews.
(ACQSC 2022)
Antibiotic Use Under the Strengthened Aged Care Quality Standards
Standard 5: Clinical Care - Outcome 5.2: Preventing and controlling infections in clinical care under the strengthened Aged Care Quality Standards (Action 5.2.1) requires aged care providers to establish an antimicrobial stewardship system that is in line with contemporary, evidence-based practice and is appropriate for the service context (ACQSC 2024).
What is Antimicrobial Resistance?
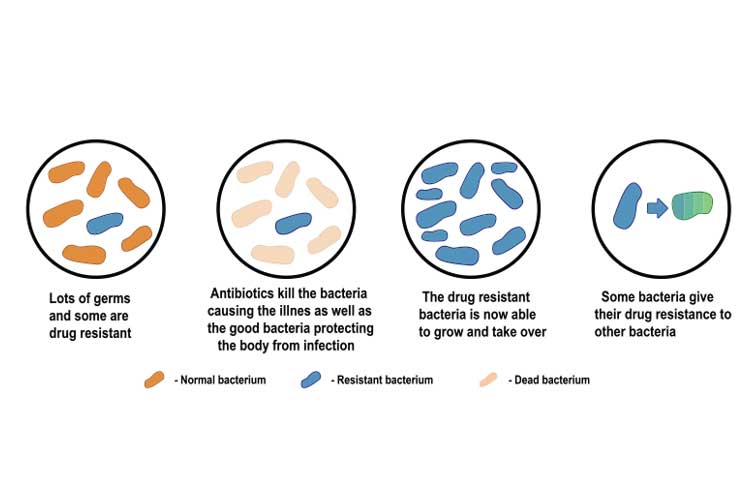
Antimicrobial resistance describes the way in which a pathogen (in this case, bacterium) may change upon exposure to an antimicrobial medication, causing it to develop a resistance to that particular medication. The medication used to treat the infection consequently becomes ineffective (WHO 2021).
These infections are notoriously difficult to treat and may result in prolonged hospital stays, disease or death. They can affect anybody and may eventually become impossible to treat (WHO 2021; CDC 2022; Australian Government 2022a).
Of particular concern are multi-resistant organisms (MROs) (colloquially known as ‘superbugs’), which are pathogens that have become resistant to several types of antimicrobials and may become untreatable by existing medicines (WHO 2021).
There is a direct link between antimicrobial resistance and the misuse or overuse of antibiotics. Antimicrobial resistance is a naturally-occurring phenomenon, however, inappropriate antibiotic use accelerates this process (WHO 2021).
In order to reduce the risk of resistant infections emerging and spreading, we must use antibiotics only when they are most needed and perform infection-prevention practices to minimise the likelihood of contracting infections in the first place (Australian Government 2022a).
What Causes Antibiotic Resistance?
- Internal resistance processes being activated by bacteria when they come into contact with antibiotics
- Bacteria changing to protect themselves from antibiotics
- Bacteria passing on resistant genes to other bacteria
- Over-prescription of antibiotics to people and animals
- People not taking antibiotics as directed
- Resistant bacteria being spread through overseas travel
- Poor hygiene and lack of infection control.
(Australian Government 2022c)
Antibiotic Misuse in Aged Care
Despite the widespread use of antibiotics in aged care, there is minimal evidence to guide antimicrobial stewardship in these facilities (Australian Government 2022d).
It may come as no surprise, then, that there are significant issues surrounding the use of antibiotics in aged care.
The 2020 Aged Care National Antimicrobial Prescribing Survey yielded some concerning statistics:
- Around 76% of residents who were prescribed antimicrobials were not displaying signs or symptoms of an infection
- 39.2% of antimicrobials had been administered for a period of over six months
- Prescription documentation was often incomplete, with only 46.2% of antimicrobials having a documented review or stop date and 23.3% of antimicrobials being administered without a recorded indication.
(DoHaAC 2023)
Why is antibiotic overuse so prevalent in aged care? Some of the identified reasons include:
- Inexperienced staff
- Lack of training in antibiotic use
- Lack of onsite medical or pharmacy staff
- Lack of infection control guidelines.
(Australian Government 2022d)
This reveals the key issue: there is a significant knowledge gap among both facilities and staff.

Appropriately Prescribing Antibiotics
It is essential to always follow antibiotic prescribing guidelines when considering antibiotics as a treatment option.
- The Therapeutic Guidelines: Antibiotic are based on the best available evidence and opinion in Australia.
- The Australian Medicines Handbook is another highly valuable resource for prescribing antibiotics.
Remember to always follow your facility’s policies and procedures.
Improving Antibiotic Stewardship in Aged Care
Antibiotic stewardship can be defined as ‘a set of commitments and actions designed to “optimise the treatment of infections while reducing the adverse events associated with antibiotic use” ’ (CDC 2021).
This is a critical skill set required by all staff involved in the prescribing and management of antibiotics.
The Antimicrobial Resistance Initiative provides the following suggestions for health professionals working in aged care:
- Instead of immediately prescribing antibiotics, consider whether there are safer alternatives.
- When prescribing antibiotics, always follow therapeutic guidelines and use diagnostics to inform decisions.
- Discuss the importance of appropriate antibiotic use and the dangers of antibiotic resistance with clients.
- Advise clients on how to manage their symptoms without antibiotics.
- Follow best-practice infection control and prevention procedures.
- Advise patients on how to prevent the spread of infections (e.g. hand hygiene).
(Australian Government 2022a)
Furthermore, the Centers for Disease Control and Prevention (2021) has developed the Core Elements of Antibiotic Stewardship for aged care. These include:
- A leadership commitment to improving antibiotic use, which includes facilitating effective communication between staff and the fostering of a workplace culture that promotes antibiotic stewardship.
- Establishing accountability for individuals involved in antibiotic prescription and management.
- Ensuring access to individuals with antibiotic expertise (e.g. pharmacists).
- Reviewing and changing policies and procedures to improve antibiotic stewardship.
- Tracking and reporting antibiotic use and outcomes within the facility.
- Ensuring all staff receive adequate education and training.
In accordance with the Therapeutic Guidelines, antibiotics should, depending on the client’s condition and clinical response, only be used for the shortest length of time possible (TG 2019).

Infection Control
One of the most important components of antibiotic stewardship is practising infection control procedures, and consequently, minimising the transmission of infections that require antibiotic treatment in the first place (Australian Government 2022e).
Facilities should be practising standard precautions for infection prevention and control, including:
- Hand hygiene
- PPE
- Safe use and disposal of sharps
- Appropriate reprocessing of reusable medical equipment and instruments
- Regular environmental cleaning
- Respiratory hygiene and cough etiquette
- Aseptic Non Touch Technique
- Appropriate waste management
- Appropriate linen handling
- Vaccination.
(Australian Government 2022e)
Managing Multi-resistant Organisms in Aged Care
If an older person is colonised with an MRO but is not experiencing any signs or symptoms of infection:
- The use of standard precautions alone is appropriate as long as the person can manage their own personal hygiene
- The person should be encouraged to perform hand hygiene before group activities or communal dining.
(ACSQHC 2024)
If an older person has an active MRO infection:
- Both standard and contact precautions need to be followed
- Aged care workers should perform hand hygiene and don gloves and gowns/aprons when providing care to the person
- Single-use or dedicated equipment should be used
- The person should be placed in a single room if possible and unnecessary movement around the facility should be reduced
- Surfaces and equipment that are in close proximity to the person or likely to be in contact with other people should be cleaned and disinfected regularly
- Infected wound sites should be covered, and wound dressings need to be changed frequently
- Continence should be appropriately managed
- The person, as well as others, should be encouraged to perform hand hygiene before and after group activities
- Isolating the person in their room is not appropriate as it could harm their social, mental and physical health.
(ACSQHC 2024)
Conclusion
While antibiotics are necessary for treating certain infections, Australian aged care facilities are suffering from significant training gaps that lead to antibiotic overuse, and, consequently, may expose their vulnerable clients to antibiotic-resistance infections.
In order to appropriately prescribe and manage antibiotics in aged care settings, it is essential to follow the best available guidelines, as well as your facility’s policies and procedures.
Test Your Knowledge
Question 1 of 3
Finish the sentence. Antimicrobial resistance occurs when ...
Topics
Further your knowledge
References
- Aged Care Quality and Safety Commission 2024, Standard 5: Clinical Care, Australian Government, viewed 14 May 2024, https://www.health.gov.au/resources/publications/strengthened-aged-care-quality-standards-august-2025?language=en
- Aged Care Quality and Safety Commission 2022, Guidance and Resources For Providers to Support the Aged Care Quality Standards, Australian Government, viewed 10 July 2023, https://www.agedcarequality.gov.au/resources/guidance-and-resources-providers-support-aged-care-quality-standards
- Australian Commission on Safety and Quality in Health Care 2024, The Aged Care Infection Prevention and Control Guide, Australian Government, viewed 6 September 2024, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/aged-care-infection-prevention-and-control-guide
- Australian Government 2022d, Antimicrobial Stewardship, Australian Government, viewed 10 July 2023, https://www.amr.gov.au/what-you-can-do/aged-care/antimicrobial-stewardship
- Australian Government 2022a, For Aged Care, Australian Government, viewed 10 July 2023, https://www.amr.gov.au/what-you-can-do/aged-care
- Australian Government 2022e, Infection Prevention and Control, Australian Government, viewed 10 July 2023, https://www.amr.gov.au/what-you-can-do/hospitals/infection-prevention-and-control
- Australian Government 2022c, What Causes AMR?, Australian Government, viewed 10 July 2023, https://www.amr.gov.au/about-amr/what-causes-amr
- Australian Government 2022a, What is AMR?, Australian Government, viewed 10 July 2023, https://www.amr.gov.au/about-amr/what-amr
- Australian Government Department of Health and Aged Care 2023, Antimicrobial Prescribing in Australian Residential Aged Care Facilities: Results of the 2020 Aged Care National Antimicrobial Prescribing Survey, Australian Government, viewed 10 July 2023, https://www.amr.gov.au/resources/antimicrobial-prescribing-australian-residential-aged-care-facilities-results-2020-aged-care-national-antimicrobial-prescribing-survey
- Centers for Disease Control and Prevention 2022, About Antibiotic Resistance, U.S. Department of Health & Human Services, viewed 10 July 2023, https://www.cdc.gov/drugresistance/about.html
- Centers for Disease Control and Prevention 2021, The Core Elements of Antibiotic Stewardship for Nursing Homes, U.S. Department of Health & Human Services, viewed 10 July 2023, https://www.cdc.gov/longtermcare/prevention/antibiotic-stewardship.html
- Therapeutic Guidelines 2019, What’s New in Antibiotic 16, Therapeutic Guidelines, viewed 10 July 2023, https://www.tg.org.au/wp-content/uploads/DownloadableWhatsNewAntibiotic2019.pdf
- World Health Organisation 2021, Antimicrobial Resistance, WHO, viewed 10 July 2023, https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
Additional Resources
- Standard 5: Clinical Care
- Stronger Standards, Better Aged Care Program | ACQSC
- The Aged Care Infection Prevention and Control Guide | ACSQHC
- Antimicrobial Resistance Initiative
- The Core Elements of Antibiotic Stewardship for Nursing Homes | Centers for Disease Control and Prevention
- National Centre for Antimicrobial Stewardship


