What is Artificial Rupture of the Membranes (ARM)?
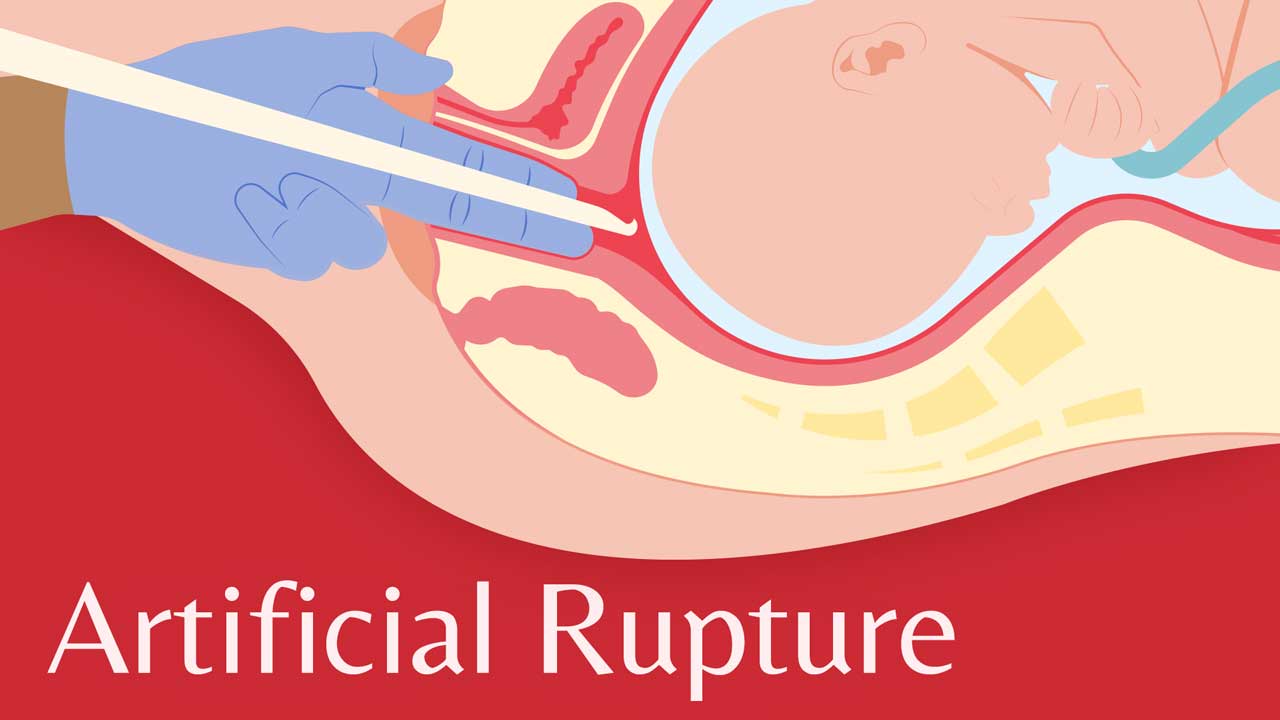
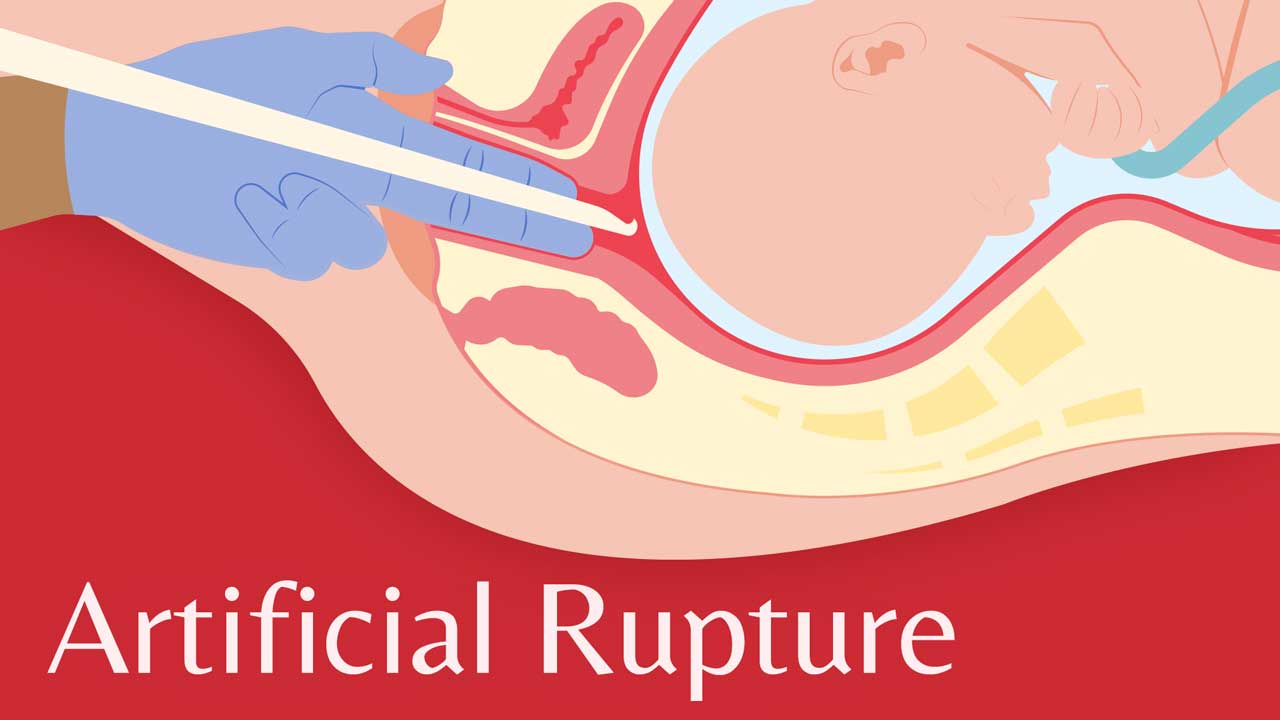
Artificial rupture of the amniotic membranes (ARM) is a method of inducing labour. It involves puncturing the membranes with a crochet-like, long-handled hook during a vaginal examination, releasing the amniotic fluid (RANZCOG 2021).
It is a simple procedure performed when the cervix is partially dilated and effaced, with the fetus in a vertex presentation with the head or other presenting part well-applied to the cervix to avoid prolapse of the umbilical cord (BHS 2019).
It’s thought that rupturing the membranes releases chemicals and hormones that can stimulate and speed up contractions and consequently shorten the length of labour (O'Connell 2021).
ARM may also be performed to allow the placement of fetal scalp electrodes if enhanced monitoring is required (Mahdy et al. 2023).
ARM may be used on its own or together with oxytocin therapy. If oxytocin is used, the fetus needs to undergo continuous cardiotocography monitoring (SCV 2023).
Note that ARM that can cause a significant increase in pain as the baby’s head will press directly on the cervix for the remainder of the labour (Cleveland Clinic 2022).
Does ARM Shorten Spontaneous Labour?

Although it’s commonly believed that ARM augments labour, there is limited evidence to support this, and data has shown mixed results. Despite this, ARM in conjunction with oxytocin has been shown to reduce the rate of cesarean birth if performed as an early intervention (Mahdy et al. 2023).
Indications for ARM
ARM might be performed to augment labour if:
- The pregnancy has extended beyond 41 weeks gestation
- The fetus is unwell or not growing well
- There are maternal health issues.
(The Women’s 2018)
Contraindications for ARM
ARM should not be performed if:
- Vasa praevia is known or suspected
- Vaginal delivery is contrainidcated
- The presenting part is unengaged.
(O'Connell 2021)
Risk Factors for ARM
Risk factors associated with ARM include:
- Maternal or neonatal infection
- Umbilical cord prolapse
- Abnormal Fetal heart rate
- Disruption of an occult placenta previa or vasa previa with subsequent maternal haemorrhage.
(SA Health 2021)
Labour Becomes More Painful With ARM

Perhaps one of the greatest arguments against ARM is that patients report it makes labour more painful. In a large study conducted by the National Childbirth Trust and reported on by the Royal College of Midwives (2012), 3,000 women were surveyed. The results were unequivocal with two-thirds of women reporting an increase in the rate, strength and pain of contractions following rupture of the membranes.
Not only did these women find their contractions more difficult to cope with, but they also needed more analgesia and felt that the physiology of labour had been disturbed, leaving them feeling less satisfied with their labour overall (RCM 2012).
Post-procedure Care
After ARM is performed, the following will need to be monitored:
- Maternal haemodynamic status
- Vital signs
- Signs of infection
- Signs of cord prolapse
- Fetal heart rate
- The quantity, colour and odour of the amniotic fluid.
(Mahdy et al. 2023; Royal Hospital for Women 2020)
Topics
References
- Ballarat Health Services 2019, Fetal Surveillance – Fetal Scalp Electrode Application (FSE), BHS, viewed 27 July 2023, https://www.bhs.org.au/bhsapps/govdoc/gdhtml/gdcpp0487-26247-55678.pdf
- Cleveland Clinic 2022, Amniotomy, Cleveland Clinic, viewed 28 July 2023, https://my.clevelandclinic.org/health/treatments/24270-amniotomy
- Mahdy, H, Glowacki, C & Eruo, FU 2023, ‘Amniotomy’, StatPearls, viewed 28 July 2023, https://www.ncbi.nlm.nih.gov/books/NBK470167/
- O'Connell, NG 2021, Amniotomy, Medscape, viewed 27 July 2023, https://emedicine.medscape.com/article/1997932-overview
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists 2021, Induction of Labour, RANZCOG, viewed 27 July 2023, https://ranzcog.edu.au/wp-content/uploads/2022/06/Induction-labour-pamphlet.pdf
- Royal College of Midwives 2012, Evidence Based Guidelines for Midwifery-Led Care in Labour: Rupturing Membranes, RCM, viewed 17 May 2020, https://www.rcm.org.uk/media/2275/evidence-based-guidelines-rupturing-membranes.pdf
- Royal Hospital for Women 2020, Artificial Rupture of the Membranes (ARM), New South Wales Government, viewed 28 July 2023, https://www.seslhd.health.nsw.gov.au/sites/default/files/documents/artificalrupturemembranes2020.pdf
- Safer Care Victoria 2023, Induction of Labour, Victoria State Government, viewed 27 July 2023, https://www.safercare.vic.gov.au/clinical-guidance/maternity/induction-of-labour
- SA Health 2021, Induction and Augmentation of Labour, Government of South Australia, viewed 28 July 2023, https://www.sahealth.sa.gov.au/wps/wcm/connect/ac7d37804ee4a27985598dd150ce4f37/Induction+and+Augmentation+of+Labour_PPG_V9_0.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-ac7d37804ee4a27985598dd150ce4f37-ocQLhIl
- The Women’s 2018, Induction of Labour, The Royal Women’s Hospital, viewed 28 July 2023, https://www.thewomens.org.au/images/uploads/fact-sheets/Induction-of-labour-181018.pdf