Clients living with diabetes may need to have their blood glucose level (BGL) monitored and kept within a target range. Maintaining an appropriate BGL is critical in reducing the risk of diabetes-related complications (Diabetes Australia 2025a).
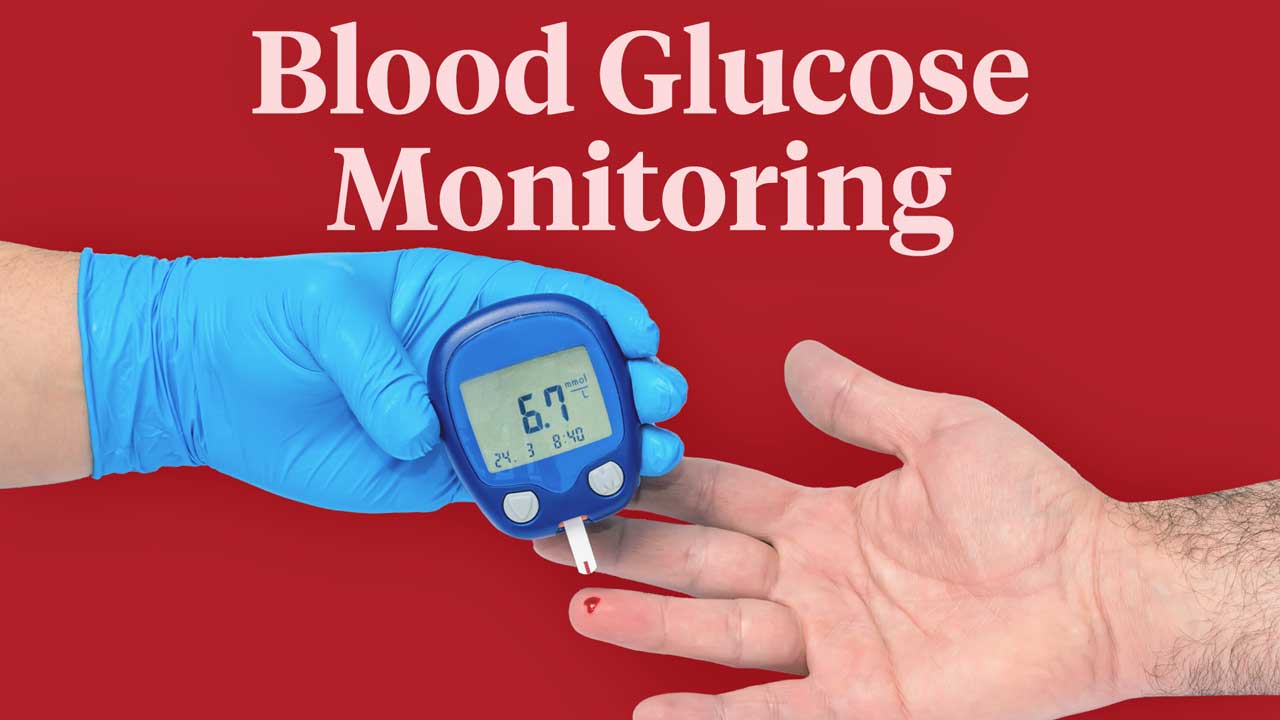
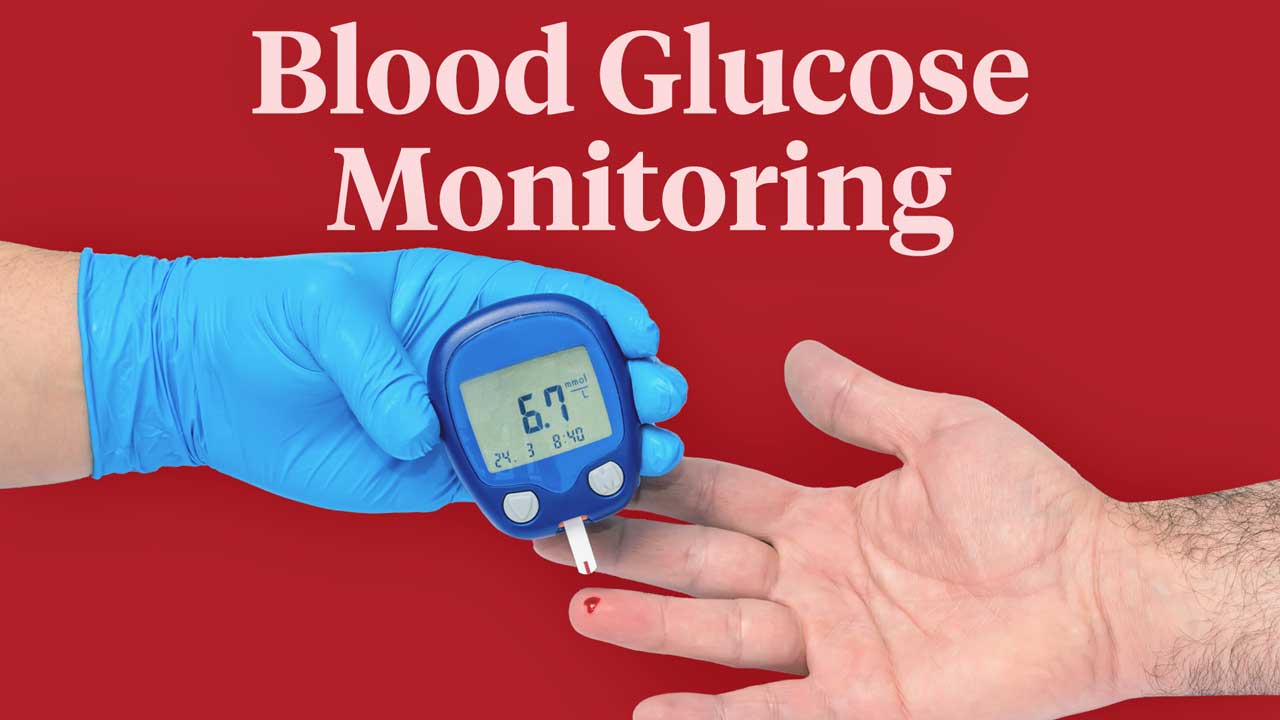
Blood Glucose Monitoring Equipment

To monitor a client’s BGL, you will need the following equipment:
- Blood glucose meter
- Lancet device with lancets
- Blood glucose monitoring strips.
(Diabetes Australia 2025a)
When Should Blood Glucose Levels be Monitored?
This should be decided by an appropriately qualified medical practitioner. Depending on the client, you may need to check their BGL at certain times, such as:
- Before breakfast
- Before lunch or dinner
- Two hours after a meal
- Before bed
- Before exercise
- When they are feeling unwell.
(Diabetes Australia 2025a)
How to Monitor Blood Glucose Levels
- Instruct the client to wash their hands in warm, soapy water (do not use hand sanitiser) and dry them thoroughly (to remove contaminants).
- Perform hand hygiene and don gloves.
- Choose the testing site. Ideally, this should be the side of the fingertip on the middle or ring finger.
- Insert the monitoring strip into the blood glucose meter.
- Prick the chosen testing site with the lancet.
- Wipe the first drop of blood away using a clean tissue or gauze, as it may contain other fluids that will contaminate the sample.
- Add a small drop of blood onto a blood glucose checking strip.
- Put the glucometer down and apply a clean tissue or gauze to the puncture site, applying pressure to manage the bleeding if required.
- The blood glucose meter will then display the client’s blood glucose level in millimoles per litre of blood (mmol/L).
- Immediately dispose of the lancet in a sharps container.
- Remove gloves and perform hand hygiene.
(Diabetes Australia 2022a; Mathew et al. 2023)
Blood Glucose Targets
Once you have tested the client’s BGL, you should check to make sure that the reading falls within the target range.
Note: The following targets are a guide only. Each client should have a suitable target recommended by an appropriately qualified healthcare professional. Always refer to your organisation’s policies and procedures first.
| Fasting/before meals | Two hours after starting meals | |
|---|---|---|
| Type 1 diabetes | 4 - 7 mmol/L | 5 - 10 mmol/L |
| Type 2 diabetes | 4 - 7 mmol/L | 5 - 10 mmol/L |
(RACGP 2024; NDSS 2021)
Document these readings and report to the appropriate clinical care staff if they are outside the target ranges.

Equipment Troubleshooting
The blood glucose meter may stop working properly for several reasons, including:
- Being too hot or cold
- Being too old
- Being exposed to moisture or humidity
- Dead batteries or battery failure
- Damaged or out-of-date testing strips
- Using the wrong type of testing strip
- Having an inadequate amount of blood on the testing strip
- Putting the testing strip in the wrong way
- The client’s hands are contaminated by dirt or food, which may interfere with the reading
- The client is experiencing dehydration or anaemia, which may reduce the accuracy of readings.
(Healthdirect 2024; Mayo Clinic 2023)
The following strategies may help to prevent equipment issues:
- Always read and follow the manufacturer’s instructions.
- Ensure that both you and the client wash your hands before performing the test. If using wet wipes, ensure the site dries completely before performing the procedure. Do not use hand sanitiser.
- Check that you’re using the correct type of testing strip.
- Ensure that you insert the testing strip correctly.
- Ask for help from colleagues if needed or contact the manufacturer’s helpline.
(Healthdirect 2024; Mayo Clinic 2023)
When to Escalate Care
The following symptoms may indicate a deterioration in the client’s health and require escalation of care to your responding clinical support team.
Signs that a client with diabetes may be experiencing hypoglycaemia (where BGL is too low) are a BGL of 4.0 mmol/L or lower (NDSS 2021), as well as any of the following symptoms:
- Weakness, trembling or shaking
- Dizziness or lightheadedness
- Sweating
- Headache
- Hunger
- Irritability or aggression
- Difficulty concentrating
- Numbness or tingling near the fingers, face or lips
- Anxiety or fear
- Slurred speech
- Confusion
- Reduced coordination
- Reduced consciousness or loss of consciousness
- Seizures
- Sleeping before meals (in older people)
- Cognitive and behavioural changes (in older people)
- Falls (in older people).
(VIC DoH 2023)
Signs that the client may be experiencing hyperglycaemia (BGL is too high) include:
- Excessive thirst
- Passing frequent, large volumes of urination
- Fatigue
- Blurred vision
- Infection
- Unplanned weight loss.
(Diabetes Australia 2022b)
Infection Control
BGL monitoring poses a risk of transmitting bloodborne viruses such as hepatitis B virus (HBV), hepatitis C virus (HCV) and human immunodeficiency virus (HIV) (CDC 2024).
In order to prevent infection transmission, you should:
- Never use the same lancet device for multiple clients, even if the needle is changed and the device is cleaned and disinfected
- Change gloves if you come into contact with lancet wounds or objects that are potentially contaminated with blood. Do this before touching any clean surfaces
- Use an alcohol-based hand rub or soap and water:
- If your hands become visibly soiled
- After you finish contact with a client
- After coming into contact with blood or body fluid
- Before touching equipment that is intended to be used for other clients
- Immediately discard used lancet devices into a sharps container after use
- Always change your gloves and perform hand hygiene between attending to different clients
- Clean and disinfect the blood glucose meter after every use (refer to the manufacturer’s instructions)
- Ensure the blood glucose meter is approved for use on multiple people before using it on another client
- Follow equipment cleaning and disinfection procedures.
(Minnesota DoH 2018; CDC 2024)
Sharps and Waste Disposal

Read: Healthcare Waste: Collection, Storage and Disposal
Lancets must always be disposed of into a designated sharps container. Never discard them into a general rubbish bin (Diabetes Australia 2025b). Testing strips should be discarded into an appropriate body fluids bin provided by your organisation.
Note: This article is intended as a guide only for non-clinical staff who are required to monitor blood glucose levels in home care clients and should not replace best-practice care. Always refer first to your organisation's policies and procedures on blood glucose monitoring.
Test Your Knowledge
Question 1 of 3
What is the correct order of steps when using a blood glucose meter to test BGL?
Topics
References
- Centers for Disease Control and Prevention 2024, Considerations for Blood Glucose Monitoring and Insulin Administration, U.S. Department of Health and Human Services, viewed 26 June 2025, https://www.cdc.gov/injectionsafety/blood-glucose-monitoring.html
- Diabetes Australia 2022a, Diabetes Quick Guides: Monitoring, Diabetes Australia, viewed 26 June 2025, https://www.diabetesaustralia.com.au/wp-content/uploads/220145-Diabetes-Quick-Guides_monitoring.pdf
- Diabetes Australia 2022b, Hyperglycaemia – Symptoms, Risks and Management, Diabetes Australia, viewed 26 June 2025, https://www.diabetesaustralia.com.au/blog/hyperglycaemia/
- Diabetes Australia 2025a, Blood Glucose Monitoring, Diabetes Australia, viewed 26 June 2025, https://www.diabetesaustralia.com.au/living-with-diabetes/managing-your-diabetes/blood-glucose-monitoring/
- Diabetes Australia 2025b, Safe Disposal of Sharps, Diabetes Australia, viewed 27 June 2025, https://www.diabetesaustralia.com.au/resources/safe-sharps/
- Healthdirect 2024, Diabetes Testing and Monitoring, Australian Government, viewed 26 June 2025, https://www.healthdirect.gov.au/diabetes-testing-and-monitoring
- Mayo Clinic 2023, Blood Glucose Monitors: What Factors Affect Accuracy?, Mayo Clinic, viewed 26 June 2025, https://www.mayoclinic.org/diseases-conditions/diabetes/expert-answers/blood-glucose-monitors/faq-20057902
- Mathew, TK, Zubair, M & Tadi, P 2023, ‘Blood Glucose Monitoring’, StatPearls, viewed 26 June 2025, https://www.ncbi.nlm.nih.gov/books/NBK555976/
- Minnesota Department of Health 2018, Checklist to Ensure Safe Injection Practices During Blood Glucose Screening, Minnesota Department of Health, viewed 27 June 2025, https://www.health.state.mn.us/facilities/patientsafety/injectionsafety/glucoseischeck.pdf
- National Diabetes Services Scheme 2021, Blood Glucose Monitoring Fact Sheet, NDSS, viewed 26 June 2025, https://www.ndss.com.au/living-with-diabetes/management-and-care/blood-glucose-monitoring/
- The Royal Australian College of General Practitioners 2024, Management of Type 2 Diabetes: A Handbook for General Practice, RACGP, viewed 26 June 2025, https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/management-of-type-2-diabetes/introduction
- Victoria Department of Health 2023, Hypoglycaemia: Standardised Care Process, Victoria State Government, viewed 26 June 2025, https://www.health.vic.gov.au/residential-aged-care/standardised-care-processes