Whether your patient is 25 or 85 years old, when they report chest pain, you should always treat it seriously.
Maybe the cause of the chest pain is nothing more than indigestion, a muscle strain or some other innocuous problem. However, chest pain can potentially point to a more serious and life-threatening cause, such as an acute myocardial infarction (AMI).
For this reason, chest pain must always be considered cardiac in nature until proven otherwise.
This article has been updated to reflect the Australian Clinical Guideline for Diagnosing and Managing Acute Coronary Syndromes 2025.
Note: This article is intended as a refresher and should not replace best-practice care. Always refer to your facility’s policy on addressing chest pain.
Making an Accurate Chest Pain Assessment
One of the most important skills available to the healthcare worker in this situation is the ability to perform an accurate pain assessment to determine whether the pain is cardiac in nature. Just as important, is the ability of the healthcare worker to conduct this assessment in a calm and controlled manner.
There are many different ways of assessing chest pain, however, one of the most popular is the PQRST pain assessment tool.
PQRST Pain Assessment Tool
P - Provoking Factors
- Where is the pain? Can you point to it?
- What provoked the pain?
- What makes the pain better?
- What makes the pain worse?
- What were you doing when the pain started?
- Did the pain occur at rest or during exertion?
- Does the pain change with repositioning?
Tip: Repositioning tends not to change chest pain caused by an AMI. If repositioning improves the pain, perhaps the issue is of musculoskeletal origin, pleuritic or pericarditis (where the pain is sometimes relieved by sitting up and leaning forward). Women who experience AMI often present with other symptoms such as dyspnoea, fatigue, nausea, diaphoresis or vomiting in addition to chest pain (Mehta et al. 2016; Brieger et al. 2025).
Q - Quality
- Can you describe the pain or discomfort?
- Is it dull, sharp, squeezing, pressure, burning, aching, pounding, cramping, stabbing or crushing?
Tip: Many patients experiencing an AMI will report chest pain (Brieger et al. 2025). However, sometimes the pain is atypical or even absent (a silent myocardial infarction) (Mankad 2024). It must be remembered that every patient is different and they will not all present with the classic substernal chest pain.
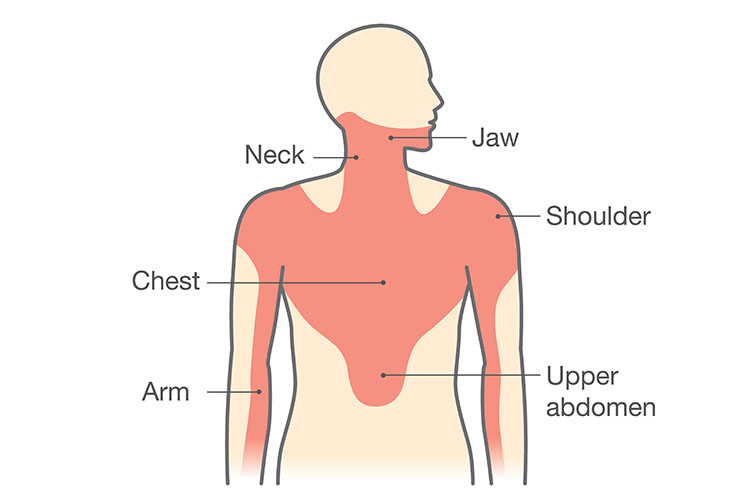
R - Radiation
- Does the pain radiate?
- To what areas?
- Does it feel like it is moving around or is localised to one spot?
- Can you point to it?
Tip: Roughly 65% of patients with an AMI will experience radiating pain (Granot et al. 2019). Common sites include the anterior chest, shoulders, arms, neck and jaw. Some patients describe jaw pain as a dull ache or a toothache, while others may describe the radiation as a band around the ribs.
S - Severity/Symptoms
- Can you rate the pain out of ten? (0 being no pain experienced and 10 being excruciating pain)
- Are you experiencing any other symptoms?
Tip: Accompanying symptoms of an AMI may include nausea, vomiting and diaphoresis. The patient may also experience dizziness and hypotension (Heart Foundation 2025a).
T - Time
- How long have you had the pain for?
- Was the onset slow or sudden?
- Is the pain intermittent (starts and stops) or is it continuous (ongoing)?
- Have you had the pain previously?
- Is it the same as last time, or different?
Tip: Angina is typically short-lived and lasts 3 to 5 minutes if the precipitating factor is relieved, such as exercise (Heart Foundation 2025b; Heart & Stroke 2025). Pain associated with AMI is not usually intermittent, though it can be.
I Think the Chest Pain May Be Cardiac in Nature… What Now?
There are a few important principles that need to be considered when managing cardiac-related chest pain. Firstly, the heart is a muscle that needs its own blood supply. The harder the heart works, the more oxygen it requires. Basically, we want to increase oxygen supply to the heart and reduce oxygen demand (Zefari 2019).
Goal-Directed Oxygen Therapy
In regards to oxygen therapy, the Australian Clinical Guideline for Diagnosing and Managing Acute Coronary Syndromes 2025 state that:
- Oxygen therapy should be provided routinely if the patient’s oxygen saturation falls below 90%.
- Oxygen therapy is often administered when oxygen saturation is 90 to 92%.
- Take caution for patients with chronic obstructive pulmonary disease (COPD), aiming for a target arterial oxygen saturation (SaO2) of about 88 to 92%.
(Brieger et al. 2025)
Coronary Vasodilators (Nitrates)
Nitrates act on vascular smooth muscle, producing a vasodilator effect on the veins and arteries, which, in turn, reduces intracellular calcium levels and leads to vasodilation.
Nitroglycerine (e.g. glyceryl trinitrate (GTN)), is often indicated in the setting of cardiac-related chest pain as it dilates the coronary vessels, improving coronary perfusion and oxygen supply to the heart (AMH 2025a; Brieger et al. 2025).
Note: GTN has several contraindications, including its use by a patient with hypotension (Brieger et al. 2025). Always check your health institution’s policy regarding GTN administration.
Antiplatelet Aggregators (Aspirin)
Aspirin may be prescribed (if not contraindicated) in the setting of chest pain to reduce the risk of thrombus formation in blood vessels (Brieger et al. 2025). Aspirin reduces the formation of thromboxanes, which mediate vasoconstriction and platelet aggregation (AMH 2025b).
Rest, Reassure and Relieve Pain
In the setting of severe chest pain, opioid analgesia (fentanyl or morphine) may be considered (Brieger et al. 2025).
Always refer to the patient’s doctor/prescriber’s advice regarding analgesic prescription and administration.
What Else Should I Do?
- Perform and document vital signs, including the ‘PQRST’ pain assessment.
- Inform senior staff immediately.
- Perform a 12-lead ECG and have it checked by a medical officer as soon as possible.
- Performing and interpreting a 12-lead ECG is a vital assessment in the setting of chest pain. An ECG will help the medical team determine if and when a patient requires reperfusion therapy to treat the cause of the chest pain.
- Nurses may be encouraged to review a 12-lead ECG with an experienced clinician to identify ECG changes that indicate a patient experiencing an ischaemic event. It is imperative that a medical officer, cardiologist or intensivist reviews the ECG. Always ensure you are treating the clinical signs and symptoms of the patient to maximise oxygenation and perfusion to the myocardium. It is suggested that a nurse should obtain a previous ECG conducted on admission or previous cardiac event.
- Ensure easy access to a defibrillator.
- Maintaining access to a defibrillator is a priority in the acute management of chest pain (Brieger et al. 2025). This is because access to a defibrillator avoids early cardiac death caused by reversible arrhythmias. Patients who are having an AMI can have associated arrhythmias.
- Senior medical staff may then order diagnostic blood tests such as a full blood examination (FBE), troponin, biochemistry and electrolytes.
- Lastly, diagnostic blood tests may be ordered. This commonly includes testing a patient’s troponin levels. Troponin is a cardiac enzyme or marker of ischaemia/infarction.
Important: The new clinical guidelines state that initial clinical assessment of ACS including history, physical examination, ECG findings and troponin testing are unable to exclude a diagnosis of ACS by themselves and patients with suspected ACS should always be referred for a complete and accurate diagnosis (Brieger et al. 2025).
Conclusion
An accurate assessment of a patient’s chest pain helps identify the likely cause and leads to prompt and appropriate responses to alleviate the pain and treat the cause. Maintaining a calm and controlled environment is essential not only for the patient’s comfort but also for yours!
Test Your Knowledge
Question 1 of 3
When should oxygen therapy be routinely administered in suspected ACS?
Topics
References
- Australian Medicines Handbook 2025a, Glyceryl Trinitrate, AMH, viewed 10 April 2025, https://amhonline.amh.net.au/chapters/cardiovascular-drugs/drugs-angina/nitrates/glyceryl-trinitrate
- Australian Medicines Handbook 2025b, Aspirin (Antiplatelet), AMH, viewed 10 April 2025, https://amhonline.amh.net.au/chapters/blood-electrolytes/antiplatelet-drugs/other-antiplatelet-drugs/aspirin-antiplatelet
- Brieger, D, Cullen, L, Briffa, T et al. 2025, ‘National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand: Comprehensive Australian Clinical Guideline for Diagnosing and Managing Acute Coronary Syndromes 2025’, Heart, Lung and Circulation, vol. 34, no. 4, viewed 10 April 2025, https://www.heartlungcirc.org/article/S1443-9506(25)00163-5/fulltext
- Granot, M, Dagul, P & Aronson, D 2019, ‘Resting Blood Pressure Modulates Chest Pain Intensity in Patients with Acute Myocardial Infarction’, Pain Reports, vol. 4, no. 3, viewed 10 April 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6749909/
- Heart Foundation 2025a, What is a Heart Attack?, Heart Foundation, viewed 10 April 2025, https://www.heartfoundation.org.au/bundles/your-heart/heart-attack
- Heart Foundation 2025b, What is Angina?, Heart Foundation, viewed 10 April 2025, https://www.heartfoundation.org.au/bundles/your-heart/angina
- Heart and Stroke 2025, Angina, Heart and Stroke Foundation of Canada, viewed 10 April 2025, https://www.heartandstroke.ca/heart-disease/conditions/angina
- Mankad, R 2024, Silent Heart Attack: What are the Risks?, Mayo Clinic, viewed 10 April 2025, https://www.mayoclinic.org/diseases-conditions/heart-attack/expert-answers/silent-heart-attack/faq-20057777
- Mehta, LS et al. 2016, ‘Acute Myocardial Infarction in Women’, Circulation, vol. 133, no. 9, viewed 10 April 2025, https://www.ahajournals.org/doi/10.1161/CIR.0000000000000351
- Zafari, AM 2019, Myocardial Infarction Treatment & Management, Medscape, viewed 10 April 2025, https://emedicine.medscape.com/article/155919-treatment#d1

