Communication Skills
A guide to practice for healthcare professionals.
 32mPublished: 11 November 2019
32mPublished: 11 November 2019



Effective communication is a skill all healthcare professionals need, but one that not all are naturally good at.
In a single day, healthcare workers can speak to people of varying educational, cultural and social backgrounds and they must do so in an effective, caring and professional manner.
This communication skills guide to practice will explore several common communication scenarios that you may find yourself in, and help you navigate and master each interaction you have in your day-to-day practice.
Chapters
Patient Communication and Building Rapport Communicating with Older Patients Communicating with Children Multidisciplinary Collaboration and Communication Communicating with Dying Patients Communicating with Patient Families and Friends Dealing with Difficult People Body Language and Non-Verbal Communication Communication Tips SummaryChapter 1
Patient Communication and Building Rapport
How to Build Patient Rapport
Choose an appropriate time to formally introduce yourself. Avoid approaching someone when they are distracted, for example during a favourite television program, or if they are stressed about an unrelated procedure.
Breaking the Ice
Break the ice by talking about the small things. Self-disclosure is unfamiliar territory for some people, while others might not have the vocabulary to describe how they feel, may not see the relevance of mentioning it, may expect judgment, or might fear they are overwhelming the other person.
Think about broaching small, less emotionally charged topics at first, as a way of opening the door to more significant conversations.
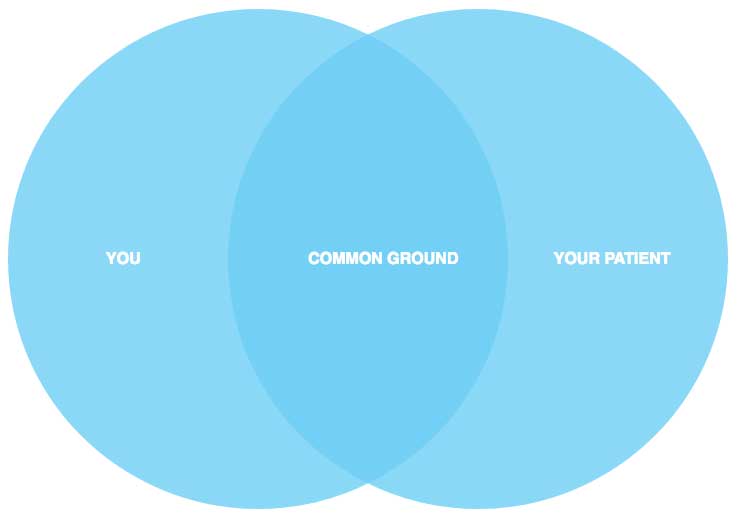
You may not have a lot of time in a shift to begin a meaningful conversation with every single patient, but for many long-stay patients, having a familiar face and some common ground between the two of you can make all the difference to their length of stay.
Consider Your Environment
Remember: time and place. Take a moment to consider your environment. Approaching a patient in a busy, high-stimulus area with lots of people can hinder your communication.
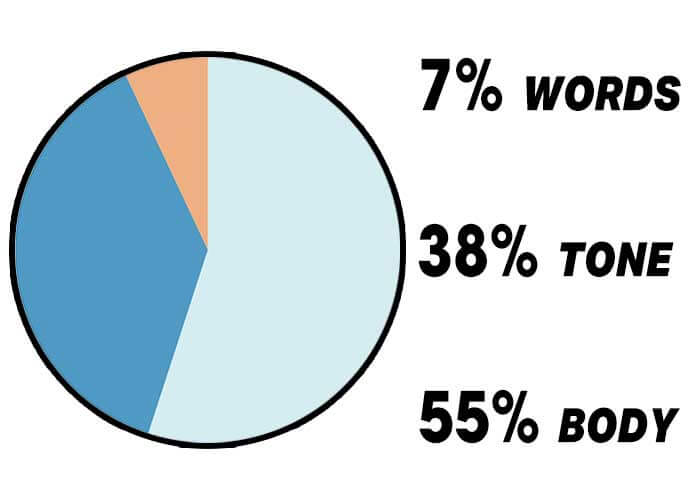
Being in a loud, chaotic emergency department may require you to raise your voice. This is problematic given that the tone of your voice makes up roughly 40% of face-to-face communication (Mehrabian 1971). Instead, it should be used to help alleviate a patient’s distress.
Loud chaotic environments also increase the chances of you, a patient or colleague mishearing important information.
If you are going to be asking questions of a personal nature, environment is particularly important. Emergency department cubicles, and beds in multi-bedded rooms are often only separated by a curtain. If you plan on asking a patient about their drug history or HIV status, for example, then finding a more private environment is essential.
Consider Technology
Whilst modern mobile technology has brought with it the benefits of instant connection, it can also be a distraction.
Ideally, when engaging with a patient you should not be taking calls. If, however you need to, it’s a good idea, out of respect to the patient, to let them know at the beginning of an interaction that you may need to take an urgent call, and apologise in advance if it is to happen.
Nurses, for example, will often carry their own personal mobile phones on their person. This can obviously have benefits such as accessing nursing apps to provide immediate medication information, for example. Be aware, however, that studies have shown the mere presence of your switched-off smart phone can be a drain on productivity (Ward et al. 2017). Consider first if you need your phone before beginning an interaction with your patient.
Most organisations have their own policies regarding technology in the workplace, it may be worth finding out what yours is.
Approaching Difficult Conversations
If you have something important to talk to them about, and the time does not seem right, fire a ‘warning shot’ by saying, “There’s something I want to talk to you about. I know you are busy but could we catch up properly in 15 minutes time?”
Listen and ask questions. Listening without interrupting is powerful. It conveys interest and respect for another’s point of view. Maintain eye contact and offer encouraging remarks such as, “I see what you are saying…” and “go on…”
Open-ended questions provide the most potent way of understanding another person. Use questions beginning with ‘why’, ‘what, ‘when’, ‘where’ and ‘how’.
Consider
Let's consider asking a patient about safe sex:
Closed-ended question:
"Do you practice safe sex?"
Open-ended question:
“Tell me how you practice safe sex?”
In some exceptionally difficult circumstances – such as the journey of a patient with cancer or someone close to death – people may feel pressured to start to talk about meaningful subjects and intimate thoughts and feelings.
For those who have avoided open communication so far, this is confronting and enormously challenging.
Communicating about difficult issues is much easier if the small steps have been taken first.
Open Discussions
Try to use the valuable time you have now to open discussion slowly.
Don’t be afraid to assert yourself when you need to by using ‘I’ statements. Being assertive involves expressing your own thoughts and feelings without dismissing or abusing the rights of others (which is aggression).
For example, saying: “I feel disappointed that you’re talking like that to me,” is a less accusatory way of expressing your feelings than, “You make me so cross when you’re so rude.”
Chapter 2
Communicating with Older Patients
Addressing older patients can be slightly different to talking to other adult-aged patients.
It is common for many older adults to have a fear of creating a fuss (Daniel 2014) – and along with a higher chance of memory and cognitive disturbances – this can create an enormous potential for missed care.
Be Patient
One of the most important considerations when communication with older adults is allowing them time. Showing any signs of stress or impatience could cause them to shut down and close off from you.
It is important to show your patient respect, regardless of their age or cognitive ability, and dedicate the right amount of time to allow them to express themselves, so to get the whole story.
Another challenge you may encounter when communicating with some older people is that they may not feel comfortable speaking openly with medical professionals, like doctors. If you are their nurse, and available for their concerns, they may be more willing to talk to you than to the doctor, who may only spend five minutes in the room.
You might find out something vital to the care and comfort of that patient just by spending a few extra minutes with them.
Watch Your Language
Using complicated medical terminology, or ‘jargon’, isn’t a good way to talk to any patient, but it is particularly detrimental when speaking with the older patient. Be mindful to put things so they are easy to understand, but without coming across as condescending.
Try to use language that is simple, clear and non-threatening, while staying honest and true. Base your language on the questions put to you and the cognitive ability of the patient you are speaking with.
Be prepared to repeat yourself and express concepts in several different ways to make sure your message is understood.

A Group Effort
Including the family is often a big part of communicating with older adults. If a family member is taking the reins in their older relative’s care, remember not to ignore the patient receiving the care.
Always try to keep your older patient in the conversation. Although a lot of what you talk about may not be understood, it is important to show them the respect and dignity of including them in the conversation, and by extension, their care.
It may help to have a three-way conversation between the patient, their carer, and yourself. When everyone works together to help the patient understand, you stand a much better chance of putting him or her at ease with all that is happening around them.
Case Study One
Carolyn is a 72-year-old female patient with a history of mild to moderate Alzheimer’s disease. Although she is forgetful, she is still able to live a relatively independent life.
She experienced an episode of fainting at Church, that was witnessed by several people, and she was taken to her primary care physician.
It took a great deal of talking to her to help Carolyn understand that the fainting spell was, in fact, a major health issue that needed to be investigated.
In addition to restricting her driving privileges, Carolyn needed several tests to rule out different probable causes of her fainting spell. Each test needed to be carefully explained to Carolyn and the information repeated.
She wrote down all the key information in a system that she had developed to keep herself from forgetting important points. In the end, she had her tests, however, doctors are still trying to determine the cause of her fainting spells.
It takes careful reminding to keep her from driving her car or performing other actions that may put her in danger.
Chapter 3
Communicating with Children
Communicating effectively with children and younger patients is one of the most difficult aspects of healthcare.
Not only are you trying to explain a difficult concept to a young person in terms they can understand, you also need to include their parents as well.
Allaying Fears
Compared with adults, children have fewer coping mechanisms and it is natural for a child to be scared, and even resistant to some medical treatment.
Explaining the procedure to a child can help to reduce anxiety and build the their confidence (Burke 2016).
As with older adults, avoid using complicated medical terminology, or ‘jargon’. Your language should be developmentally appropriate. Make a mental note of the patient’s age and their level of understanding, and tailor your speech to meet their needs.
Avoid the use of negative words, such as ‘hurt’ and ‘sting’. Offer lots of reassurance, perhaps in the form of a small reward for their resilience and bravery.
You may need to moderate your language, get down to the level of the child, and use a positive and non-threatening tone of voice to show them that you mean no harm.
As with most communication, careful listening, as well as showing your patient you are listening through positive body language, will serve you well in talking to children patients.
Distraction
Distraction techniques have been shown to be effective in reducing pain and distress during medical procedures in children (Duff et al. 2011).
The Royal Children’s Hospital (2016) offers a great resource for tailoring appropriate diversion techniques to a child’s age, including the use of toys, singing, and breathing and relaxation. Find The Royal Children’s Hospital Non-Pharmacological Methods of Pain Management at their website.
Procedural Pain Management
Fact SheetThe Royal Children's Hospital – Psychological Interventions PDF
Parents
A large part of communicating with children patients is the inclusion of their parents or guardians.
You are likely to deal with some people who are in a great deal of distress. Try to allay their fears as best you can, answering all their questions as honestly as possible.
Never lie and be sure to refer them to the right person if you don’t know the answer to a question.
Some parents may get emotional and you need to be aware of possible angry or sorrowful outbursts. Outbursts such as these can upset your patient, which may go against what you are trying to accomplish.
Try removing the parents away from the child when holding particularly difficult or emotional conversations. Employ active listening techniques, as you would for any other patient and their family.
Case Study Two
Daniel is a two-year-old heart patient who is preparing for his second open-heart surgery. He doesn’t understand what has to happen to him, and the atmosphere of the hospital room makes him scared. Already, starting the IV line has been a traumatic event.
One of the nurses from the OR visits Daniel’s room the night before the operation with a bag of items. She gets down on her knees with Daniel and shows him the hair net he will be wearing, the tubes that will help him breathe, and the mask that would be placed over his face.
Instead of being afraid, Daniel is now fascinated by the new toys in front of him and plays with them. During this time, the nurse takes a moment to talk to the parents about any concerns they have. She helps them to understand the procedure, the heart-lung machine, and the estimated time of the surgery.
When the nurse prepares to leave after half an hour, both Daniel and his parents are much more at ease. Although all of them are still nervous about the surgery, getting familiar with the process and tools for the procedure has helped calm Daniel so that he – and his parents – can get some much needed rest before his operation.
Chapter 4
Multidisciplinary Collaboration and Communication
Your patient’s condition is deteriorating and you need to tell the doctor. You have their vitals, their chart, and a full head of information that you want to blurt out as soon as the doctor’s voice crackles across the phone line.
It’s important to not be overwhelmed by the sheer amount of information you need to communicate to a potentially very busy member of the health team.
Methodically working through what you need to communicate will help you to remember each point and to deliver it in a time efficient manner.
To do this, one of the best-practice and most widely used handover tools is the iSoBAR framework.
What is iSoBAR?
iSoBAR is a standardised mnemonic to improve clinical communication. It stands for identification, situation, observation, background/history, agree to a plan (actions) and responsibility and risk management.
(Australian Commission on Safety and Quality in Health Care 2017)Identification
First, introduce yourself and identify who you are, your role, and who you are talking about (your patient or client). Be sure to use at least three patient identifiers.
Situation
Name the reason for your call, the reason for the patient’s admission, or the type of incident that has taken place, e.g. the patient has fallen. Provide current diagnosis, concerns or other critical information.
Observation
Check, update and discuss recent vital signs and observations. If appropriate, don’t be afraid to insert your own assessment at this stage, such as you are worried about the patient, or that they don’t ‘look right’ to you.
Background History
Update and discuss relevant medical and support information. Offer the basics of the patient’s relevant history. Include the timeline leading up to the situation, e.g. what was the patient doing earlier in the day that may have impacted the situation?
Provide all relevant clinical assessments such as pathology, recent test data, and any other collected information relating to the patient background.
Agree to a Plan (actions)
Outline a plan for assessment, treatment and eventual discharge.
Recommending a solution to the situation may involve a request for further tests, for example. Trust your assessment skills and the knowledge you have collected about your patient’s condition when recommending a course of action to another team member.
If handing over, this offers the new team member a clear course of action to follow or opens up the lines of communication for further discussion.
Responsibility and risk management
Confirm your shared understanding of what is to be done. Clarify each person’s tasks (read back any critical information to check understanding). Conclude handover.
Did you know?
There are several other examples of similar mnemonic tools used to structure handover, including:
- ISBAR (Identify, Situation, Background, Assessment, Recommendation);
- SBAR (Situation, Background, Assessment, Recommendation);
- SHARED (Situation, History, Assessment, Risk, Expectation, Documentation);
- I PASS the BATON (Introduction, Patient, Assessment, Situation, Safety concerns, Background, Actions, Timing, Ownership, Next).
Chapter 5
Communicating with Dying Patients
Among the most difficult scenarios that can arise for caregivers when communicating with patients is talking with a patient who is dying.
It is uncomfortable and emotionally challenging to face a person who has just received a prognosis without hope, and who you know will be facing their biggest struggle - not only physically, but mentally and spiritually.
Self Care
It is important for you to be in a healthy mental state when working with a population of patients who are in the process of dying. This means taking care of yourself and allowing yourself time to disconnect from work.
When you go home, you need to leave the sadness and emotion of the job at work. Carrying these feelings everywhere with you may make you susceptible to compassion fatigue - a syndrome that can lead to depression, anger and the breakdown of relationships.
Honesty
Don’t pretend that everything is fine. The patient deserves the respect of you acknowledging their situation, and not doing so can make them feel as if you are infantilising them. However, do not allow yourself to be overcome with emotions either.
Continue to give the same honest, loving care you have been providing the patient. Tend to their needs and answer their questions as best you can.
Watch: Active and Empathic Listening
Being Present
Your patient may also need to open up to someone and trusts you because you are their nurse or carer. Sometimes in this situation, words are not needed.
Communication can be about quietly projecting the energy that you are here, you are willing to listen, and you won’t judge. That is the best therapeutic gift you can give your patient.
Read the social cues. If they need you to be present, be present. If they are tired of talking, give them the space they need.
Chapter 6
Communicating with Patient Families and Friends
In most care settings, healthcare professionals will be communicating with a patient’s family and friends on a regular basis.
Navigating these interactions pragmatically is best; be aware of the nuances of inter-family politics that may exist.
Appointing a Family Representative
You may spend a great deal of time turning people down in their hunt for information.
Although it should be the responsibility of the immediate family to manage extended members and friends, this job can often fall to the nurse on shift.
Often in large family situations, a representative should be appointed as the main contact. This way, the nurse only has to explain a situation once. Ideally, it should be the next of kin. Sometimes families may want a member with a medical background to handle updates and check-ins.
Though you are not in charge of the family, you may occasionally need to step in and make suggestions that they may or may not comply with. If they don’t comply, it may be necessary to call a family meeting and explain the importance of a contact person.
Explaining that the blurring of these clear communication lines can affect their loved one's care can be an effective way of communicating this.
Your assertiveness as a nurse will be put to the test in a large family situation. Stand your ground and always put the patient first. You can help minimise bad feelings by actively listening, moderating your body language and assuring friends and family that you understand they are concerned about the patient.
Honesty is, once again, very important, and you shouldn’t make empty promises to keep a relative calm. Once you have established that they are privy to the details, tell them the truth about what is going on with their loved one.
Be prepared for a wide range of reactions. Some will react with anger, but most will react with neutrality or sadness. In some cases, this can be more difficult to deal with than hostility. Offer yourself as a sounding board for the relative. Make it a point to be there for them, a presence of peace and understanding. Comfort them and do not betray their trust in you.
Patient Rights v Family Rights
Families may have the best intentions, but the patient’s rights always come first.
If relatives and friends are disturbing the patient’s rest, working them up or causing them unnecessary distress, the nurse has the right to step in and remove the family. The same rights apply to patients who are in the next bed over.
In these cases, it is important to talk to the patient and the family member. Ask the patient if they are comfortable with their family and if they would like the family to have restricted access to them. Most will decline, but at least you are offering the opportunity to the patient.
Next, talk with the family. Explain that their behaviours are upsetting the patient and that a different approach is needed. There is no reason to be falsely happy, but tell them to simply be with the patient instead of focussing on the negative, for example.
Acknowledge the fear they are feeling and offer them the same compassion you would offer your patients.
Case Study Three
Mr Reed is an 82-year-old man who has come into the intensive care unit after suffering an acute stroke.
He is the proud father of five children, all of whom are married, and a grandfather of ten. Some of these grandchildren are old enough to have spouses of their own.
Unfortunately, Mr Reed's wife died last year and his care has been transferred to his eldest daughter, Lisa.
The relationship between Lisa and her siblings is complicated, and all of them have insisted on obtaining a security code for themselves to access information about Mr Reed’s condition. Lisa, not wanting to start an argument, has given it to her brothers and sisters, who in turn, gave it to a few grandchildren.
Every day on the unit, the nurse assigned to Mr Reed receives at least five phone calls about his status. Although the nurse tries to be concise, often these conversations can take up to twenty minutes. After a few days of this, the day nurse brings the family together and explains the difficulties in handling so many calls when their father’s care is so critical.
It is decided that all information will flow through Lisa, although this does not make everyone happy. The plan is agreed to, however, and now the nurse need only field one update call per shift and continue to communicate with her elderly patient, Mr Reed.
Chapter 7
Dealing with Difficult People
Difficult personalities can be found everywhere; not only amongst our patients but within their families and coworkers, too.
Saying the wrong thing to a particular person can escalate a situation quickly and requires a caregiver to remain professional and to be assertive - not aggressive.
Retain Professionalism
Retaining professionalism is essential when these encounters escalate. Everyone has the right to let off steam, and there is nothing inherently wrong with venting to a trusted confidante, providing you find an appropriate place and time to do so. On the floor, however, professionalism is expected at all times.
To be a professional means to not forget yourself.
You are a representative of your facility and the nursing profession in general. Raising your voice, publicly gossiping or arguing in front of patients or the public has no place in the workplace.
Try to find amicable ways to solve a problem so that all parties are satisfied. This may mean compromising for the sake of peace, or involving your management and HR in the discussion, where appropriate.
Dealing With Angry Patients
Someone who is acting angry may simply be frightened, defensive or resistant to what is going on around them.
It is important for a nurse to take a step back from the patient who is angry and ask themselves what is really going on. If the patient is actually frightened, then you will have to approach them differently than if they are truly angry over something, such as a long wait time.
De-Escalating
The best course of action is to carefully interview the patient to draw out what they are feeling.
First calm yourself and take stock of your own emotions. Begin to engage the person by using reflective statements, such as “I can understand why you feel that way,” and try to discuss possible solutions with them.
Avoid accusatory or negative language, such as, “You neglected to,” which indicates they are lying, “You say that,” which makes the person seem less intelligent, “I fail to understand how,” and demanding phrases such as, “You should.”
These language gambits can lead to an escalation.
A more appropriate approach would be to use positive language to de-escalate and defuse the situation, and give the patient no opportunity to overreact.
For instance, you could say, “It seems you have a different viewpoint on this situation. Let me explain our position.”
This statement allows the patient to be heard and allows you to state your side of the argument.
Another good positive response is, “Might we suggest to you…” or, “An option open to you is…”
This allows the patient to know what their options are in a non-threatening manner.
Chapter 8
Body Language and Non-Verbal Communication
Your body language tells the story of your emotions far better than words do.
Positive-language
If you are seething with anger and attempt to use positive-language while clearly wound tighter than a drum, people will notice and will likely respond to the message coming for your body cues rather than your voice.
Take a moment to relax and control your body before engaging in a situation you expect to be heated.
Eye contact is important - it conveys honesty, openness and helps when being assertive.
Relax your facial expressions to keep from grimacing, twisting or pursing your lips, lifting your eyebrows, or scowling.
Keep your hands and arms in front of your body, not crossed. Crossing your arms sends a message that you are closed off, uninterested or confrontational.
Make use of space. If your patient is in a bed, crouch down to their level rather than towering over them. Don’t get too close, however, as this can be invasive.
Tone
‘Our tone tells the truth even when your words don't.’ (Lickerman 2010).
In his research in ‘ Silent Messages’ (1971), Professor Albert Mehrabian of UCLA, demonstrated that when words and non-verbal communication (tone and body language) are in conflict, people will almost always believe the non-verbal message.
Tone can help de-escalate a distressed and angry patient. This is referred to as the ‘emotional contagion effect’, where your emotional state can affect how another person feels.
If you approach a distressed and angry patient, raise your voice and use a forceful tone, you run the risk of escalating the patient’s distress and anger. However, if you approach the interaction with a gentle, caring tone of voice, it will very likely help to calm and defuse the situation.
Click to explore
The following diagrams illustrate four different interpersonal distances (Hall 1966):

Public distance: for public address, formal, for larger audiences.
Personal Space
Make use of space by understanding the basic principles of proxemics - or the study of personal space.
You can moderate your body language by utlising these different spaces.
For example, crouching down to a patient who is laying in bed, rather than towering over them, to offer comfort – or leaving plenty of space between you and a person who is angry or distressed, so to not only protect yourself, but to ensure the other person feels safe.
Summary
Communication Tips in Summary
Speak slowly:
Certain words sound very similar to one another if they are spoken quickly.Take the time to speak slowly and carefully to ensure your words are less likely to be mistaken by others.
Speech volume:
When communicating with some people, especially those who are older, the inclination might be to raise your voice dramatically in an effort to be understood. Instead of speaking louder, try speaking with more clarity.
Avoid slang and jargon:
A common mistake that many health professionals make is to use bigger and more complicated words. Another common mistake is the use of slang terms that are not fitting or appropriate. Avoid both of these mistakes for better communication.
Speak to your audience:
What you say to a doctor or a fellow nurse might be very different to what you would say to a patient and their family. Use the word ‘medicine’ rather than ‘drug’ when talking to patients. Many people associate the word ‘drug’ with illicit substances, whereas health professionals view the word ‘drug’ as any pharmaceutical. Choose your words to fit the situation and the audience.
Listen:
Communication is a two-way street. One of the most important communication skills is the ability to stop and listen actively and ethically, to what is being said by the other person.
Reflect:
If you are a little unclear of what someone has said, reflect by repeating what they have said in your own words, back to the person. If you have misunderstood, this gives the person a chance to clarify their meaning and shows you are actively listening.
Use body language:
The majority of human communication is understood to be through body-language (Mehrabian 1972), despite our words. Be conscious of what your body is saying and whether it is in agreement with your words. Don’t send mix messages.
Foreign Languages:
It might sound strange, but learning a new language puts you in better touch with your native tongue and can open your eyes to the way you use the words you already know.
Don’t Forget Other Methods of Communication:
In addition to speaking and listening, don’t forget that there are other skills that you should work on, such as reading, writing and technology-based communication.
- Ahern, G, 2017, ‘The Art of Active Listening’, Ausmed, viewed 13 March 2019, https://www.ausmed.com/cpd/lecture/active-listening
- Alvarado, K, Lee, R, Christoffersen, E, Fram, N, Boblin, S, Poole, N, Lucas, J & Forsyth, S 2006, ‘Transfer of Accountability: Transforming Shift Handover to Enhance Patient Safety’, Healthcare Quarterly, vol. 9, pp. 75-9, viewed 13 March 2019, http://www.longwoods.com/content/18464
- Ausmed Editorial Team 2016, ‘10 Tips to Enhance Communication at Shift Handover’, 27 October, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/tip-to-enhance-communication-at-shift-handover
- Australian Commission on Safety and Quality in Health Care 2018, ‘6. Communicating for Safety Communication at Clinical Handover: Clinical Handover Action 6.7’, NSQHS Standards, 20 May, viewed 25 June 2019, https://www.nationalstandards.safetyandquality.gov.au/6.-communicating-safety/communication-clinical-handover/clinical-handover
- Burke, N 2016, ‘Nursing Paediatric Patients - Effective Procedural Communication’, Ausmed, 29 July, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/nursing-paediatric-patients-effective-procedural-communication
- Duff, A, Gaskell, S, Jacobs, K, & Houghton, J 2012, ‘Management of Distressing Procedures in Children and Young People: Time to Adhere to the Guidelines’, Archives of Disease in Childhood, vol. 97, no. 1, pp. 1-4, doi: 10.1136/archdischild-2011-300762.
- Grohol, JM 2018, ‘Become a Better Listener: Active Listening’, PsychCentral, viewed June 2018, https://psychcentral.com/lib/become-a-better-listener-active-listening/
- Hall, ET 1966, ‘Distances in Man’, The Hidden Dimension, http://www.academia.edu/5668023/Edward_T._Hall-_The_Hidden_Dimension
- Hodgkinson, K & Gilchrist, J 2008, Psychosocial Care of Cancer Patients: A Health Professional’s Guide to What to Say and Do, Ausmed Publications, Melbourne, Victoria.
- Hodgkinson, K 2017, Talking with Children About a Parent or Guardian’s Cancer Diagnosis, Ausmed, viewed 13 March 2019, https://www.ausmed.com/cpd/courses/talking-with-children-about-cancer
- Hodgkinson, K 2015, Communicating with Patients, Ausmed, 18 May, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/communicating-with-patients
- Lampert, L 2016, ‘How to Handle Difficult Patients’, Ausmed, 6 October, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/how-to-handle-difficult-patients
- Lampert, L 2016, Communicating with Doctors, Ausmed, 28 October, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/communicating-with-doctors
- Lampert, L 2015, Communicating with Older Patients’, Ausmed, 23 March 2015, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/communicating-with-older-patients
- Lampert, L 2015, ‘Communicating with Children in Healthcare’, 26 March 2015, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/communicating-with-children-in-healthcare
- Lampert, L 2015, ‘Communicating with Dying Patients’, Ausmed, 1 June, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/communicating-with-dying-patients
- Lampert, L 2015, ‘Communicating with a Patient’s Family and Friends’, Ausmed, 13 April, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/communicating-with-a-patients-family-and-friends
- Lampert, L 2016, ‘How to Be Assertive’, Ausmed, 12 October, viewed 13 March 2019, https://www.ausmed.com/cpd/articles/how-to-be-assertive
- Lautrette, A, Darmon, M, Megarbane, B, Joly, LM, Chevret, S, Adrie, C, Barnoud, D, Bleichner, G, Bruel, C, Choukroun, G, Curtis, R, Fieux, F, Galliot, R, Garrouste-Orgeas, M, Georges, H, Goldgran-Toledano, D, Jourdain, M, Loubert, G, Reignier, J, Saidi, F, Souweine, B, Vincent, F, Barnes, NK, Pochard, F, Schlemmer, B & Azoulay, E 2007, ‘A Communication Strategy and Brochure for Relatives of Patients Dying in the ICU’, vol. 356, pp. 469-478, viewed 13 March 2019, https://www.nejm.org/doi/full/10.1056/NEJMoa063446#t=abstract
- Lickerman, A 2010. ‘The Importance of Tone: How we often communicate the opposite of what we intend’, in Psychology Today, 5 August, viewed 25 June 2019, https://www.psychologytoday.com/au/blog/happiness-in-world/201008/the-importance-tone
- Lower, SE 2008, ‘Communication Between the Nurse and Family Caregiver in End-of-Life Care: A Review of the Literature’, Journal of Hospice and Palliative Nursing, vol. 10, no. 1, pp. 35-45.
- Martin, D 2014, ‘Too polite to make a fuss: Elderly NHS patients suffer in silence say health watchdog’, in The Daily Mail, 7 April, viewed 13 March 2019, https://www.dailymail.co.uk/news/article-2598355/Too-polite-make-fuss-Elderly-NHS-patients-suffer-silence-say-health-watchdog.html
- Mehrabian, A 1971, Silent Messages, Wadsworth Publishing Company, Belmont, CA.
- Milford, PC 2018, ‘3 Tips for Talking to Children about Traumatic Events’, PsychCentral, viewed 13 March 2019, https://psychcentral.com/blog/3-tips-for-talking-to-children-about-traumatic-events/
- National Institute on Aging, National Institutes of Health & Department of Health and Human Services, Talking With Your Older Patient: A Clinician’s Handbook, viewed 13 March 2019, http://memoryworks.org/PUBS/NIA/Talking%20With%20Your%20Older%20Patient-A%20Clinician's%20Handbook.pdf
- PBS Parents 2018, Talking with Kids, PBS, viewed 13 March 2019, http://www.pbs.org/parents/talkingwithkids/
- Robinson, TE, White, GL Jr & Houchins, JC 2006, ‘Improving Communication with Older Patients: Tips from the Literature’, Family Practice Management, vol. 13, no. 8, pp. 73-8, viewed 13 March 2018, https://www.ncbi.nlm.nih.gov/pubmed/17022433
- SA Health 2016, ISBAR A standard mnemonic to improve clinical communication, Department for Health and Ageing, Government of South Australia, viewed 13 March 2019, https://www.sahealth.sa.gov.au/wps/wcm/connect/8a8b26804896068a9cb8fc7675638bd8/15111.3-+Clinical+Handover+Fact+Sheet+%28V1%29WebS.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-8a8b26804896068a9cb8fc7675638bd8-m08hRA0
- Sleeman, KE & Collis, E 2013, ‘Caring for a Dying Patient’, BMJ, vol. 346, viewed 13 March 2019, https://www.ncbi.nlm.nih.gov/pubmed/23596214
- Wake, D 2016, ‘Collaboration and Communication’, Ausmed, viewed 13 March 2019, https://www.ausmed.com/cpd/courses/collaboration-and-communication
- Ward, AF, Duke, K, Gneezy, A & Bos, MW 2017, ‘Brain Drain: The Mere Presence of One’s Own Smartphone Reduces Available Cognitive Capacity’, Journal of Association for Consumer Research, vol. 2, no. 2, viewed 25 June 2019, https://www.journals.uchicago.edu/doi/full/10.1086/691462
- Worden, JW 1991, Talking to Children About Death, Hospice, viewed 13 March 2019, https://www.hospicenet.org/html/talking.html
Social distance: impersonal, social, casual.