Working in healthcare, you may interact with and care for clients in the community (e.g. aged care and home care settings) who use CPAP machines.
This article will provide a refresher on how CPAP machines work and caring for clients using them.
What is Continuous Positive Airway Pressure (CPAP)?
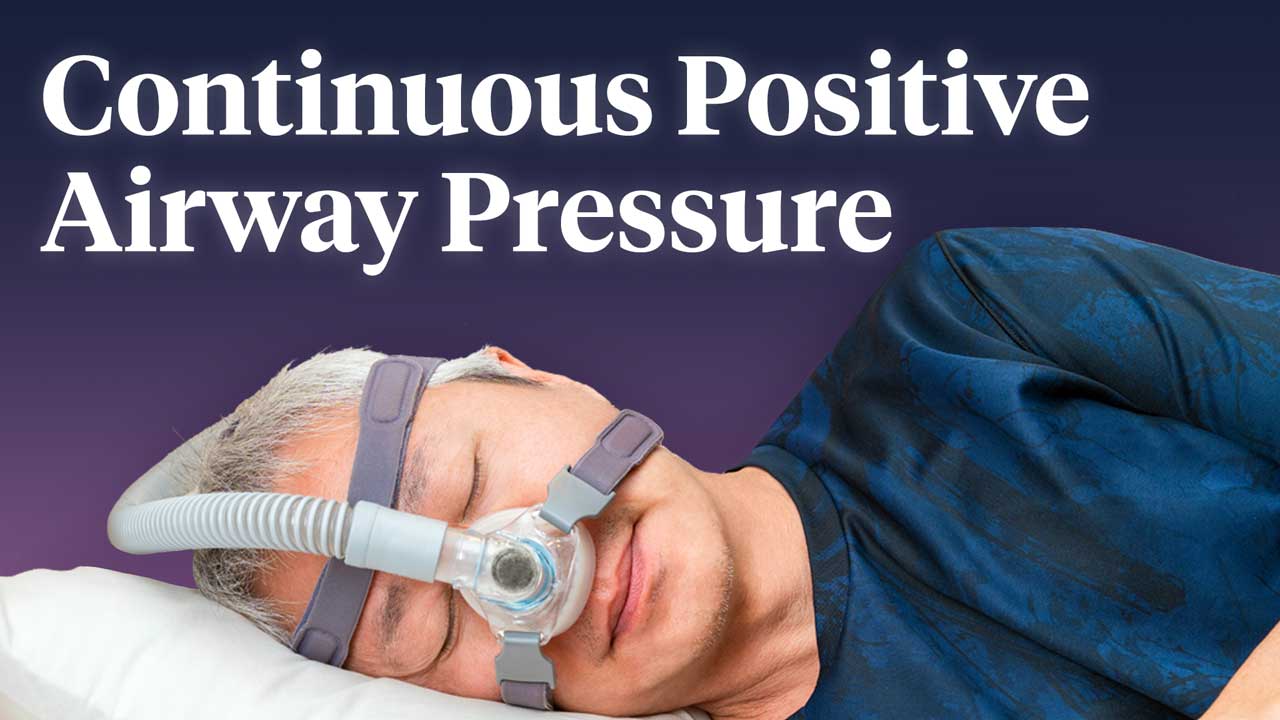
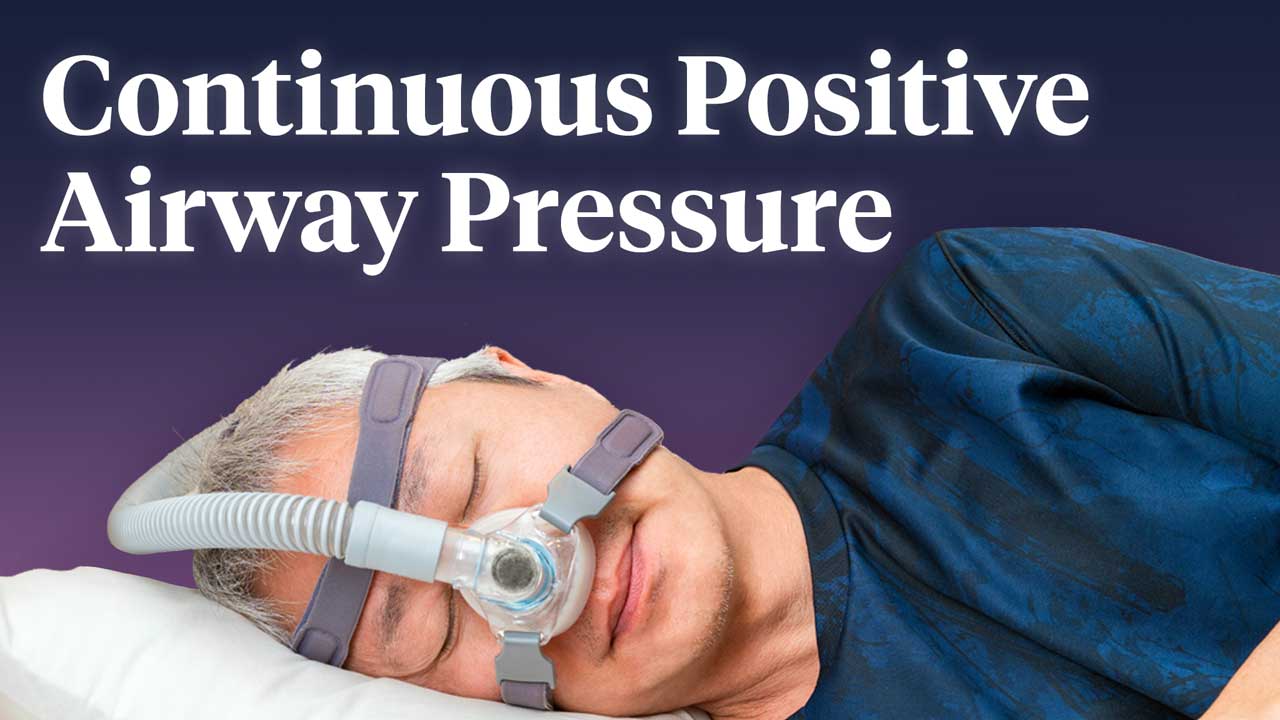
Continuous positive airway pressure (CPAP) is a type of non-invasive ventilation commonly used to treat moderate to severe obstructive sleep apnoea (OSA) (Nickson 2024; Healthdirect 2024).
A CPAP is often the first-line treatment for OSA in adults and is considered the most effective non-surgical intervention (Ignite Healthwise 2024). Clients can use a CPAP themselves in an outpatient or home setting (Pinto et al. 2025).
OSA causes partial or complete obstruction of the airway during sleep, causing the client to stop breathing, wake up and then go back to sleep. This process may repeat hundreds of times in one night (Healthdirect 2024).
Read: Obstructive Sleep Apnoea: More Than Just a Bad Night's Sleep
A CPAP machine administers a steady stream of airflow into the airway, maintaining a continuous pressure that functions as a stent to keep the airway open throughout the night (Pinto et al. 2025).
In addition to preventing the airway from collapsing, a CPAP increases the ability for oxygen to enter the lungs and fill alveoli sacs. This is where gas exchange occurs and allows carbon dioxide to be removed (GOSH 2024).
There are three components of CPAP:

- A machine to pressurise the air
- A facial mask (‘interface’) that the person wears at night
- A hose that connects the machine to the mask in order to deliver the pressurised air to the person.
(GOSH 2024; Suni 2023)
Headgear (straps or a mesh cap) holds the mask in place and creates a seal around the nose and/or mouth (GOSH 2024).
Types of CPAP Masks
A CPAP can be administered using one of several types of interfaces. It is important to determine which type of interface is most appropriate for the client’s needs:
| Type of interface | Description | May be appropriate for: | Image |
|---|---|---|---|
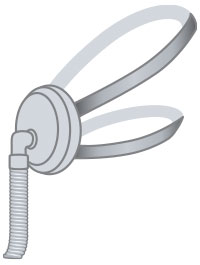
| Nasal pillow mask | A small mask that sits over the nostrils, or nasal prongs that sit directly inside the nostrils. |
|
 |
| Nasal mask (nasal continuous positive airway pressure or NCPAP) | A mask that covers the nose only. This is the most common CPAP interface. |
|
 |
| Full-face mask | A full-face mask that fits over the nose and mouth. |
|
 |
Humidifier Chambers
Humidifier Chambers
Some CPAP machines have a humidifier chamber, which moisturises the air that is being delivered to the client. This reduces side effects including mouth and throat dryness, nosebleeds, runny nose and congestion (Suni 2023; Pinto et al. 2025).
Humidification is important as the air delivered by a CPAP machine enters the airway too quickly for the nose to naturally warm it. Humidified air is more comfortable to breathe, less damaging to the tissue in the upper airway and lungs and less likely to wake the client up (ResMed 2024).
Contraindications for CPAP
Note: Escalation of care is crucial in these situations.
- Inability to breathe spontaneously
- Reduced consciousness (should not be used for those with a GCS score of 8 or less)
- Person is uncooperative or severely anxious
- Unstable cardiorespiratory status/respiratory arrest
- Facial trauma/burns
- Recent facial, oesophageal or gastric surgery
- Air leak syndrome (such as pneumothorax with bronchopleural fistula)
- Excessive respiratory secretions
- Severe nausea and vomiting
- Severe air trapping conditions with hypercarbia, such as asthma or chronic obstructive pulmonary disease (COPD).
(Pinto et al. 2025; QAS 2023)
Benefits of CPAP
The use of a CPAP may:
- Reduce the work of breathing
- Minimise the use of accessory muscles when breathing is difficult
- Improve pulmonary gas exchange
- Decrease intubation rates
- Decrease the length of hospital stays
- Reduce sleep disruptions
- Improve the quality of sleep
- Prevent snoring
- Reduce sleepiness during the day
- Reduce headaches in the morning
- Improve functioning during the day
- Improve the quality of sleep for the client’s partner.
(GOSH 2024; Ignite Healthwise 2024; QAS 2023)
Disadvantages of CPAP
- A CPAP may cause side effects, including congestion, runny nose, dry mouth, sore throat, hypotension, dry cornea, barotrauma, respiratory infections, chest discomfort, excessive dreaming (initially) and nosebleeds
- Clients may initially experience feelings of discomfort, claustrophobia or embarrassment
- The CPAP mask may cause skin redness, irritation or pressure injuries on the face
- Clients may initially experience discomfort in the morning after using the CPAP
- The CPAP mask and hose require regular cleaning, inspection and replacement every three to six months
- Clients may experience abdominal distension or bloating, which may lead to nausea, vomiting and aspiration
- Poorly fitting masks may leak
- Lack of client compliance is common. This may be due to the education they are receiving.
(Pinto et al. 2025; Ignite Healthwise 2024; QAS 2023; Suni 2023)

How to Set Up and Use a CPAP Machine
- Find an appropriate place to put the CPAP machine. It should be on a stable surface, close to the bed, close to a power outlet and have unobstructed access from the bed. Nightstands and bedside tables are good choices.
- Check the filter (see the written instructions).
- Attach the hose to the machine, using the special connector. The hose should stay in place easily.
- Plug the hose into the mask. It should fit tightly and may click into place.
- If the CPAP has an attached humidifier, fill it with distilled water up to the maximum fill level.
- Plug the CPAP machine into a power outlet.
- Put the mask over the face, then attach or pull the straps to secure it into place. This should create a seal without pinching the skin. Adjust the length of the straps if needed.
- Turn on the device (an appropriately qualified healthcare worker should have already set the correct pressure settings).
- Tighten the mask if you hear air escaping.
(Suni 2023)
How to Clean a CPAP Machine
Note: Always refer to the manufacturer’s instructions.
- Mask:
- Wipe cushion daily with a damp cloth
- Clean cushion and frame weekly, rinse thoroughly and allow to air dry
- Handwash headgear as required
- Ventilation tubing: Clean once per week, rinse thoroughly and allow to air dry
- Humidifier chamber:
- Replace water daily
- Clean once per week with a vinegar and water solution, rinse thoroughly and allow to air dry
- Ventilator and humidifier housing: Damp dust weekly
- Air inlet filter: Replace whenever it becomes discoloured (generally every three months).
(GOSH 2024)

Caring for Clients Who Use a CPAP Machine
The following practical tips may help you care for clients who use a CPAP machine:
- Understand that clients may take a while to adjust to the CPAP at first
- Always exercise patience and empathy, and provide thorough, gentle education around the implementation of the device
- If the client is resistant to using the CPAP, determine what exactly they dislike, e.g. the mask or the pressure
- Encourage clients to use the CPAP every time they sleep
- Encourage anxious clients to try relaxation techniques before using the CPAP, or to practice using the mask while they are awake
- Encourage the client to wash their face prior to using the CPAP, as this will assist in creating a seal and help to prevent skin irritation
- Ensure the client’s mask fits properly, and consider trying different interfaces that may be more suitable
- Consider using a CPAP machine with a ‘ramp’ feature, which allows air pressure to gradually increase as the client falls asleep
- Consider a nasal saline spray for clients who are experiencing a dry or stuffy nose
- If the client has a habit of unintentionally removing the mask during the night, consider setting an alarm to check that it is still on
- Encourage the client to avoid caffeine and alcohol before bedtime so that they are able to fall asleep more easily
- Ensure the mask is clean and dry before the client wears it.
(Suni 2023; Mayo Clinic 2024b; GOSH 2024)
The Importance of Client Education
Appropriate client education is crucial in ensuring compliance, and, subsequently, long-term success. It’s important to monitor the client’s compliance, especially when they are first commencing CPAP therapy, as many people stop treatment prematurely due to discomfort (Pinto et al. 2025).
Encourage clients to inform you of any adverse effects they are experiencing and ensure these are addressed by an appropriately qualified clinician. It’s also important to make sure that the CPAP machine is checked regularly and the mask fits properly (Pinto et al. 2025).
In addition to providing continuing client education on the benefits of regular CPAP use, clients should also be encouraged to take other measures to improve the effectiveness of treatment, including:
- Maintaining a healthy weight
- Maintaining a healthy diet
- Exercising regularly
- Avoiding smoking.
(Pinto et al. 2025)
Test Your Knowledge
Question 1 of 3
How often does a CPAP mask and hose need to be replaced?
Topics
Further your knowledge
 Free
Free Free
FreeReferences
- Great Ormond Street Hospital for Children 2024, Mask Ventilation/ Non-Invasive Ventilation (NIV), NHS Foundation Trust, viewed 18 June 2025, https://www.gosh.nhs.uk/conditions-and-treatments/procedures-and-treatments/non-invasive-ventilation/
- Healthdirect 2024, Obstructive Sleep Apnoea (OSA), Australian Government, viewed 18 June 2025, https://www.healthdirect.gov.au/sleep-apnoea
- Mayo Clinic 2024a, Which CPAP Masks Are Best For You?, Mayo Clinic, viewed 19 June 2025, https://www.mayoclinic.org/diseases-conditions/sleep-apnea/in-depth/cpap-masks/art-20546828?s=1
- Mayo Clinic 2024b, CPAP Machines: Tips For Avoiding 10 Common Problems, Mayo Clinic, viewed 25 June 2025, https://www.mayoclinic.org/diseases-conditions/sleep-apnea/in-depth/cpap/art-20044164
- Ignite Healthwise 2024, Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea, University of Michigan Health, viewed 18 June 2025, https://www.uofmhealth.org/health-library/hw48752
- Nickson, C 2024, Non-Invasive Ventilation (NIV), Life in the Fast Lane, viewed 18 June 2025, https://litfl.com/non-invasive-ventilation-niv/
- Pinto, VL, Sankari, A & Sharma, S 2025, ‘Continuous Positive Airway Pressure’, StatPearls, viewed 18 June 2025, https://www.ncbi.nlm.nih.gov/books/NBK482178/
- Queensland Ambulance Service 2023, Clinical Practice Procedures: Respiratory/Non-Invasive Ventilation - CPAP, Queensland Government, viewed 19 June 2025, https://www.ambulance.qld.gov.au/clinical/cpm/procedures
- Resmed 2024, ‘Why Use a CPAP Humidifier?’, Resmed Sleep Blog, 20 November, viewed 19 June 2025, https://www.resmed.com/en-us/sleep-apnea/sleep-blog/why-use-a-cpap-humidifier/
- Suni, E 2023, How to Use a CPAP Machine for Better Sleep, Sleep Foundation, viewed 19 June 2025, https://www.sleepfoundation.org/cpap/how-to-use-cpap-machine