Endometriosis affects about one in nine Australians assigned female at birth - about 830,000 people (Tsirtsakis 2022).
What is Endometriosis?
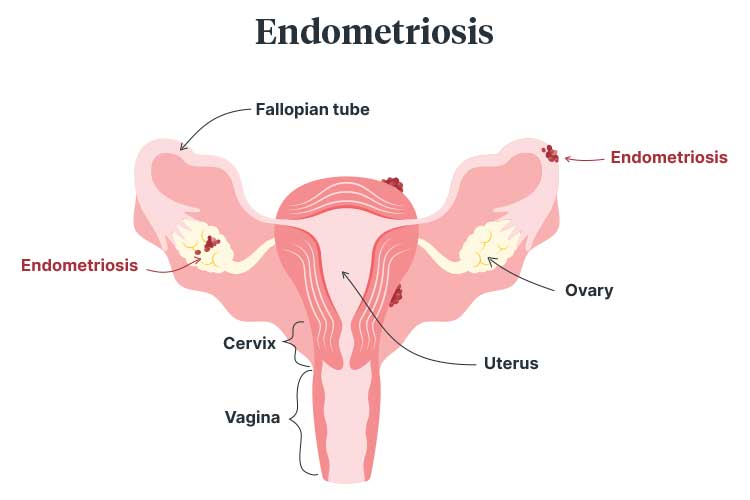
Endometriosis is a condition where tissue similar to the endometrium (lining of the uterus) grows outside of the uterus. This usually occurs in the pelvis, but it’s possible for endometriosis to affect almost any part of the body (Healthdirect 2023).
The cause of endometriosis is not entirely clear (Healthdirect 2023).
The dominant theory is that during menstruation, menstrual tissue (comparable to lining in the womb) passes back through the fallopian tubes and into the pelvis, where it attaches and grows (The Women’s 2020).
It’s believed that this stray tissue (known as endometrial implants or lesions) continues to behave as it would inside the uterus. It thickens, breaks down and bleeds with each menstrual cycle. Because the stray tissue can’t leave the body as normal menstrual blood would, it remains inside the pelvis and causes inflammation (Sparks 2019; Healthdirect 2023).
People who have endometriosis often report experiencing crippling pain. It has the potential to impact a person’s relationships, capacity to work and study, physical health and mental wellbeing (WHO 2023).
Endometriosis appears to run in families. If a person’s mother or another close relative has endometriosis, it’s more likely they will develop it too (The Women’s 2020).
Endometriosis is sometimes found in people who are not able to fall pregnant. In a small sample of these people, scar tissue caused by endometriosis is blocking the fallopian tubes (The Women’s 2020).
Risk Factors for Endometriosis
While the reasons why certain people experience endometriosis are unclear, there appear to be factors that increase the likelihood of developing it.
- Beginning to menstruate at an age earlier than 11
- Experiencing menopause at an older age
- Experiencing short menstrual cycles (e.g. less than 27 days)
- Extended, heavy menstrual periods
- Never giving birth
- Being a lower body weight
- Having higher oestrogen levels
- Family history of endometriosis
- Any abnormalities to the reproductive tract.
(Mayo Clinic 2023)
Symptoms of Endometriosis
Symptoms may include:
- Menstrual pain
- Pain during sex
- Pelvic pain outside of the menstrual cycle
- Back pain
- Leg or thigh pain
- Heavy periods
- Bleeding between periods
- Bladder or bowel bleeding
- Changes in urination or bowel movements
- Bloating
- Lethargy
- Pain while passing a bowel motion.
(The Women’s 2020; Healthdirect 2023)
People who have endometriosis often report the difficulty of getting their pain under control even after medical intervention, including surgery (Sinclair & Armour 2019).

Self-Management Techniques
To highlight how severe the pain of endometriosis is, a 2019 study revealed that among participants aged 18 to 45, the percentage of people who reported using self-management techniques for endometriosis in the past six months was 76% (Sinclair et al. 2019).
These self-management techniques included:
- Heat packs (70%)
- Altering diet (44%)
- Exercise (42%)
- Yoga or pilates (35%)
- Cannabis (13%).
(Sinclair & Armour 2019)
Diagnosing Endometriosis
A laparoscopy (keyhole surgery) or open surgery is required to make a definitive diagnosis of endometriosis. A laparoscopy involves making a very small incision in the abdomen and inserting a laparoscopic telescope to look inside the body. A small sample of tissue will be taken and a biopsy will then confirm the diagnosis (The Women’s 2020; Healthdirect 2023).
Unfortunately, endometriosis is often underdiagnosed in Australia, with an average delay to diagnosis of 6.4 years (O’Hara et al. 2020).
The underdiagnosis of endometriosis is related to factors such as:
- Variation in symptoms between patients
- The need for an invasive procedure to make a formal diagnosis
- Societal stigmas about menstruation
- Lack of education about menstrual health.
(DoH 2018)
Treating Endometriosis
There is currently no cure for endometriosis, but there are a variety of treatment options (Healthdirect 2023).
Pharmacological treatments may include hormone-based therapies such as oral contraceptives, an implant or IUD, or analgesics. As hormones cause endometriosis lesions to undergo a similar cycle to a woman’s menstrual cycle, hormone therapies can be effective when treating endometriosis symptoms (NICHD 2020).
Surgical treatments aim to remove the presence of endometriosis as much as possible. There are multiple options available. These include:
- Laparoscopic surgery (as mentioned above) to facilitate examination and removal of tissue.
- Laparotomy, a type of open surgery
- Bowel surgery, which may be necessary if the endometriosis has expanded to the bowel wall
- Hysterectomy (removal of the uterus), which is performed only in severe cases.
(Better Health Channel 2022)
Some people might undergo a combination of hormone therapy and surgical treatment (Better Health Channel 2022).
It’s important to note that not all treatments work for all people, and symptoms may return once treatment is stopped (NICHD 2020).
Other Strategies
The following strategies may be helpful in reducing pain and inflammation from endometriosis:
- Pelvic floor physiotherapy
- Exercise
- Maintaining a healthy diet
- Emotional support or counselling
- Massage
- Naturopathy, herbal medicines, acupuncture or yoga.
(Better Health Channel 2022)

Conclusion
Endometriosis is a painful and, unfortunately, common condition. It has previously been linked with infertility and can cause a reduction in quality of life.
People who are experiencing symptoms of endometriosis should talk to their general practitioner regardless of whether symptoms are consistent month-by-month. There are treatments available for people who live with endometriosis.
Test Your Knowledge
Question 1 of 3
How many people does endometriosis affect?
Topics
References
- Better Health Channel 2022, Endometriosis, Victoria State Government, viewed 12 January 2024, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/endometriosis
- Department of Health 2018, National Action Plan for Endometriosis, Australian Government, viewed 12 January 2024, https://www.health.gov.au/resources/publications/national-action-plan-for-endometriosis?language=en
- Eunice Kennedy Shriver National Institute of Child Health and Human Development 2020, What are the Treatments for Endometriosis?, U.S. Department of Health and Human Services, viewed 12 January 2024, https://www.nichd.nih.gov/health/topics/endometri/conditioninfo/treatment
- Healthdirect 2023, Endometriosis, Australian Government, viewed 11 January 2024, https://www.healthdirect.gov.au/endometriosis
- Mayo Clinic 2023, Endometriosis, Mayo Clinic, viewed 12 January 2024, https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- O’Hara, R, Rowe, H & Fisher, J 2020, ‘Managing Endometriosis: A Cross-Sectional Survey of Women in Australia', Journal of Psychosomatic Obstetrics & Gynecology, vol. 43, no. 3, viewed 12 January 2024, https://www.tandfonline.com/doi/full/10.1080/0167482X.2020.1825374
- Sinclair, J and Armour, M 2019, ‘1 in 10 Women with Endometriosis Report Using Cannabis to Ease Their Pain’, The Conversation, 12 November, viewed 12 January 2024, https://theconversation.com/1-in-10-women-with-endometriosis-report-using-cannabis-to-ease-their-pain-126516
- Sparks, D 2019, ‘Women’s Wellness: Learn About Endometriosis’, Mayo Clinic News Network, 17 October, viewed 11 January 2024, https://newsnetwork.mayoclinic.org/discussion/womens-wellness-learn-about-endometriosis/
- Tsirtsakis, A 2022, ‘Doctor Education ‘Highest Priority’ for People With Endometriosis’, newsGP, 1 April, viewed 11 January 2024, https://www1.racgp.org.au/newsgp/clinical/doctor-education-highest-priority-for-people-with
- The Women’s 2020, Endometriosis - Information For Women, The Royal Women’s Hospital, viewed 11 January 2024, https://thewomens.r.worldssl.net/images/uploads/fact-sheets/Endometriosis-information-women.pdf
- World Health Organisation 2023, Endometriosis, WHO, viewed 11 January 2024, https://www.who.int/news-room/fact-sheets/detail/endometriosis