Careful thought and creativity are as important to menu planning for home care clients as they are to the selection of our own daily meals – if not, more so, given the heightened health complications inherent with ageing, disability or illness.
One of the benefits of receiving care in the community or home setting is its personalised nature, and food and meal choice is one of the most personal choices a person can make.
For this reason, our clients not only expect but have a right to provide input into the type of meals they receive.
It is well known that food consumption and nutrition are closely linked to our overall quality of life. Furthermore, studies have shown that increased independence in food choice and active participation in food planning are associated with a reduced risk of malnutrition (Abbey 2015).
This article will provide broad nutritional advice and methods of effective meal planning for home care clients.
Malnutrition in Home Care
While malnutrition is difficult to measure, it’s estimated that 15% of people receiving home care in Australia are malnourished (TAS DoH 2020).
Older people are known to be at a disproportionate risk of malnutrition (DPS Media 2017). There are many reasons for this, including:
- Decreased food intake due to factors such as isolation and reduced ability to access food
- Physical impairment such as disability, reduced appetite, reduced sense of taste or smell, difficulty chewing or swallowing, difficulty self-feeding and difficulty preparing food
- Cognitive and psychological issues such as dementia, depression, anxiety, self-neglect and bereavement
- Being unable to consume certain food groups due to difficulty chewing, swallowing or digesting
- Polypharmacy, which may impair nutrient absorption or increase nutrient loss
- Having a poor mealtime environment
- Increased nutrient requirements due to illness, infection, medications, etc.
(TAS DoH 2020; DPS Media 2017)
People living with disability or chronic illness may be at increased risk of malnutrition due to factors such as:
- Loss of appetite, nausea, vomiting or diarrhoea caused by chronic illness
- Impaired mood and reduced desire to eat caused by mental illness
- Impaired ability to digest food and absorb nutrients due to conditions such as Crohn's disease and ulcerative colitis
- Increased energy requirements due to surgery or involuntary movements (e.g. tremor)
- Taking certain medicines
- Impaired ability to mobilise, cook or shop for food.
(NHS 2023)

A Dietary Guide for Home Care Clients
Foods to Avoid
- Limit foods that are high in saturated fats, such as cakes, pastries, processed meats, pizza, fried foods and potato chips
- Limit foods and drinks with added salt, and avoid adding salt to food when eating
- Limit foods and drinks high in sugar, such as confectionery, sugar-sweetened soft drinks, cordials and fruit drinks
- Limit consumption of alcohol to no more than two standard drinks per day
- Keep 'extras' such as lollies, cakes, biscuits, fried foods and pizza to a minimum - they should not feature regularly and are not part of a healthy diet.
(Better Health Channel 2017)
Foods to Embrace
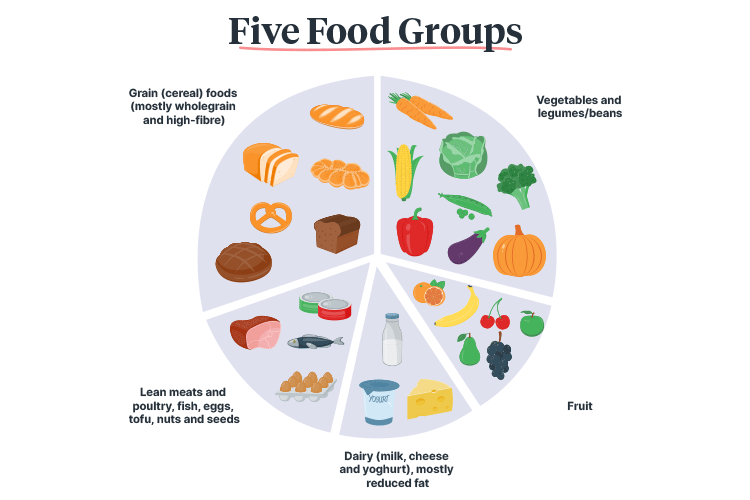
- Eat from each segment of the food group regularly:
- Vegetables, fruit, legumes and beans:
- Choose a variety of types and colours (e.g. green, orange, red, yellow, purple and white)
- Lean meats and poultry, fish, eggs, tofu, nuts and seeds
- Grain (cereal) foods (mostly wholegrain and high-fibre)
- Dairy (milk, cheese and yoghurt), preferably reduced-fat varieties
- Vegetables, fruit, legumes and beans:
- Drink plenty of water (six to eight cups every day)
- Swap foods that are high in saturated fat with foods containing polyunsaturated and monounsaturated fats
- Switch foods such as butter, cream, cooking margarine, coconut and palm oil with unsaturated fats from oil, nut-based butters and pastes, and avocado
- Eat fish regularly as it has been known to reduce the risk of heart disease, stroke, dementia and macular degeneration.
(Better Health Channel 2017; NHMRC 2013; Nutrition Australia 2021)
For recommended servings based on age and gender, see the National Health and Medical Research Council’s Australian Dietary Guidelines Summary.
Meal Planning
We eat with our eyes first, which means that the visual appearance of a meal matters. When planning meals, incorporate a wide variety of colours, textures, flavours and types of food to keep things interesting (Comcater 2024).
While rotational meals are undoubtedly a more convenient option when providing home care, remember the importance of meal variation for nutritional needs and meal enjoyment.
Meal Planning Considerations
Some clients have specific meal requirements. When planning meals, always take into account the following:
- Medical needs
- Allergies and intolerances
- Dietary restrictions (e.g. vegetarian)
- Eating and swallowing capabilities
- Cultural customs
- Religious food practices
- Mental illness
- Personal likes and dislikes
- Medicines being taken
- Additional energy requirements (e.g. due to unplanned weight loss, illness or injury)
- Overweight and obesity.
(Metro South Health 2018)

Test Your Knowledge
Question 1 of 3
True or false? Polyunsaturated and monounsaturated fats are to be avoided.
Topics
References
- Abbey, KL, Wright, OR & Capra, S 2015, ‘Menu Planning in Residential Aged Care-The Level of Choice and Quality of Planning of Meals Available to Residents’, Nutrients, vol. 7, no. 9, viewed 2 July 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4586549/
- Better Health Channel 2017, Nutrition Needs When You’re Over 65, Victoria State Government, viewed 2 July 2025, https://www.betterhealth.vic.gov.au/health/healthyliving/Nutrition-needs-when-youre-over-65
- Comcater 2024, What Makes a Great Aged Care Menu?, Comcater, viewed 2 July 2025, https://www.comcater.com.au/insights/what-makes-a-great-aged-care-menu/
- Metro South Health 2018, A Toolkit for Healthy Eating in Supported Accommodation: A Best Practice Guide, 2nd edn, Queensland Government, viewed 2 July 2025, https://www.metrosouth.health.qld.gov.au/about-us/get-involved/resources-to-build-healthier-communities/healthy-eating
- National Health and Medical Research Council 2013, Australian Dietary Guidelines: Summary, Australian Government, viewed 2 July 2025, https://www.eatforhealth.gov.au/sites/default/files/files/the_guidelines/n55a_australian_dietary_guidelines_summary_130530.pdf
- National Health Services 2023, Malnutrition, NHS, viewed 2 July 2025, https://www.nhs.uk/conditions/malnutrition/causes/
- Nutrition Australia 2021, Nutrition and Older Adults, Nutrition Australia, viewed 2 July 2025, https://nutritionaustralia.org/fact-sheets/nutrition-and-older-adults/
- DPS Media 2017, ‘Older People at Disproportionate Risk of Malnutrition’, Talking Aged Care, 30 May, viewed 2 July 2025, https://www.agedcareguide.com.au/talking-aged-care/older-people-are-often-at-disproportionate-risk-of-malnutrition
- Tasmania Department of Health 2020, Malnutrition, Tasmanian Government, viewed 1 July 2025, https://www.health.tas.gov.au/sites/default/files/2021-11/Malnutrition_factsheet_DoHTasmania2020.pdf

