Narcolepsy is a rare condition causing persistent tiredness, ‘sleep attacks’ during the day, and in some cases, muscle weaknesses that can cause a person to collapse involuntarily.
Narcolepsy is a chronic neurological condition characterised by recurring periods of excessive sleepiness. It may also cause cataplexy (sudden involuntary muscle weakness or paralysis), hallucinations and/or sleep paralysis (NINDS 2023).
Episodes of cataplexy may occur frequently and at any time, often triggered by strong emotions such as fear, anger, excitement or surprise (Brain Foundation 2024).
Narcolepsy is rare and estimated to affect about 4 in every 10,000 people worldwide, with onset generally during adolescence or early adulthood (though it can develop at any age). Symptoms may develop over a number of years (Sleep Health Foundation 2025).
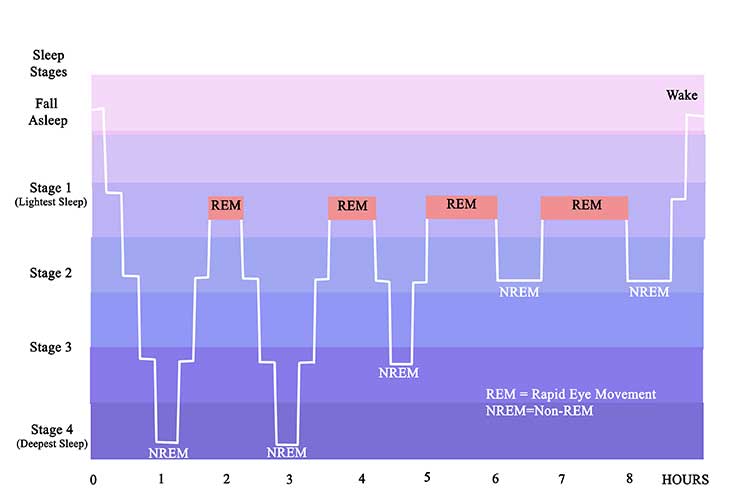
A normal night of sleep will consist of several sleep cycles, each involving one period of non-rapid eye movement (NREM) sleep, then one period of rapid eye movement (REM) sleep. REM sleep generally begins after the first 60 to 90 minutes of sleep and is the window in which dreaming will occur. During REM sleep, the muscles go limp so that the individual does not act out their dreams (NINDS 2025).
A person with narcolepsy, however, will enter REM sleep much earlier than the average person (sometimes within 15 minutes of falling asleep) and may suddenly enter REM sleep or experience the associated muscle weakness during the day, or while still awake (NINDS 2025; Brain Foundation 2024).
What Causes Narcolepsy?
Narcolepsy is caused by dysfunction of the sleep-wake regulators in the brain, though the reason why they function incorrectly in some people is not completely understood. It’s thought that a very low level of the chemical hypocretin (which regulates wakefulness) is the cause, as almost all people with narcolepsy who experience cataplexy lack normal levels of hypocretin (NINDS 2025).
However, those with narcolepsy who do not experience cataplexy usually have normal levels of hypocretin (NINDS 2025).
Risk Factors for Narcolepsy
Narcolepsy may be linked to:
- Autoimmune disorders: Lack of hypocretin is thought to be linked to abnormalities in the immune system, wherein hypocretin-producing brain cells are wrongly attacked.
- Genetics: Up to 10% of individuals with narcolepsy have a close relative with similar symptoms, but most cases have no known link to family history.
- Brain injuries, tumours or diseases may interfere with the parts of the brain that regulate wakefulness.
- Age: Narcolepsy can affect anyone but usually begins between the ages of 10 and 30.
(NINDS 2025; Mayo Clinic 2024)
Symptoms of Narcolepsy
- Excessive day sleepiness: This is the most common and obvious symptom. Even if the individual is well-rested, they will experience persistent sleepiness and ‘sleep attacks’ when they are otherwise alert.
- Cataplexy: Sudden muscle weakness, which is thought to be linked to the limpness that occurs during REM sleep. It may range from weakness in only some muscles to complete collapse. Some people experience frequent episodes, while others only experience one or two in a lifetime. Not everyone who has narcolepsy experiences cataplexy. As cataplexy occurs in very few diseases, it can be a good indicator of narcolepsy.
- Sleep paralysis, which is a temporary inability to move or speak during sleep or while waking up. Sleep paralysis usually only lasts for a brief period of time but can be distressing. People without narcolepsy can also experience sleep paralysis.
- Altered REM sleep: People with narcolepsy may enter REM sleep more quickly than usual and during the day.
- Hallucinations, which can be distressing.
- Fragmented or disrupted sleep.
- Automatic behaviour, wherein the individual falls asleep but continues the task they were in the middle of.
- Other sleep disorders such as sleep apnoea and insomnia.
(NINDS 2025; Mayo Clinic 2024; Sleep Health Foundation 2025)
Note that all people with narcolepsy experience excessive sleepiness, but will not necessarily have any other symptoms (NINDS 2023).

Diagnosing Narcolepsy
According to the DSM-5, the following criteria should be met to diagnose narcolepsy:
- Recurring periods within one day consisting of uncontrollable tiredness, lapses into sleep or napping. These should have occurred at least three times per week for the past three months, and
- Evidence of at least one of the following:
- Episodes of cataplexy at least a few times per month, or
- Proven hypocretin deficiency as measured by cerebrospinal fluid, or
- Nocturnal sleep polysomnography test demonstrating the onset of REM sleep in 15 minutes or less, or a multiple sleep latency test demonstrating an average sleep latency of 8 minutes or less and more than two sleep onset REM periods.
(PsychDB 2022)
Some diagnostic methods for narcolepsy include:
- Examination of sleep history, which can involve filling out the Epworth Sleepiness Scale test.
- Keeping a sleep diary for a certain period of time.
- Polysomnography: This is a test requiring an overnight stay at a medical facility. It involves measuring the electrical activity of the brain and heart, movement of the muscles and eyes, and breathing.
- Multiple sleep latency test: This involves taking four to five naps every two hours during the day, with a specialist monitoring how long it takes to fall asleep.
- Spinal tap, which involves obtaining a sample of the patient’s cerebrospinal fluid and measuring the level of hypocretin in the sample.
(Mayo Clinic 2024; NINDS 2025)
Treating Narcolepsy
Treating narcolepsy involves managing symptoms, as there is no cure for the condition. This may involve medication to help with sleepiness and cataplexy (Sleep Health Foundation 2022). Other strategies that may help manage symptoms include:
- Scheduling short naps throughout the day
- Keeping a regular sleep schedule
- Avoiding caffeine or alcohol before bed
- Refraining from smoking
- Exercising daily
- Avoiding heavy meals before bed
- Relaxing before bed and ensuring sleep space is comfortable.
(NINDS 2025)
It is extremely important to ensure symptoms are adequately controlled before the patient undertakes activities where sleepiness could be dangerous (e.g., driving). Advise the patient never to drive if they are feeling sleepy (Sleep Health Foundation 2025).
Test Your Knowledge
Question 1 of 3
How might narcolepsy affect someone’s REM sleep?
Topics
References
- Brain Foundation 2024, Narcolepsy, Brain Foundation, viewed 12 March 2025, https://brainfoundation.org.au/disorders/narcolepsy/
- Mayo Clinic 2024, Narcolepsy, Mayo Clinic, viewed 12 March 2025, https://www.mayoclinic.org/diseases-conditions/narcolepsy/symptoms-causes/syc-20375497
- National Institute of Neurological Disorders and Stroke 2025, Narcolepsy, U.S. Department of Health and Human Services, viewed 12 March 2025, https://www.ninds.nih.gov/health-information/disorders/narcolepsy
- PsychDB 2022, Narcolepsy, PsychDB, viewed 12 March 2025, https://www.psychdb.com/sleep/4-narcolepsy
- Sleep Health Foundation 2025, Narcolepsy, Sleep Health Foundation, viewed 12 March 2025, https://www.sleephealthfoundation.org.au/narcolepsy.html