Challenging behaviours are a common symptom of many conditions, such as intellectual disability, autism and dementia.
When poorly managed, these behaviours can have far-reaching effects, including distress for the person, disruptions to the lives and comfort of other care recipients, and added stress and workloads for healthcare workers.
BPSD: Behavioural and Psychological Symptoms of Dementia
In a home or aged care setting, the behavioural and psychological symptoms of dementia (or BPSD) are common but remain one of the biggest challenges to care staff.
Mishandling of BPSD can lead to the inappropriate use of restrictive practices, which should be a last resort for care staff, but have time and time again been incorrectly used as a frontline approach to changed behaviours.
Behaviour Management and BPSD Under the Strengthened Aged Care Quality Standards
Standard 5: Clinical Care - Outcome 5.6: Cognitive Impairment under the strengthened Aged Care Quality Standards requires aged care providers to establish processes for:
- Recognising and reducing situations that may lead to behavioural changes in older people with cognitive impairment
- Recognising and addressing causes of behavioural changes in older people with cognitive impairment, including clinical causes.
(ACQSC 2025)
Managing Behaviours: Person-Centred Approach
The following tips will provide carers with a foundational understanding of behaviour management to ensure their clients receive effective person-centred care when displaying BPSD.
There are countless ways to handle changed behaviours. However, approaching the situation methodically with an assessment tool like the ABC approach examines the behaviour from a person-centred perspective. The aim of this type of approach is to help us understand the aetiology of the behaviour and develop a suitable, consistent response for ongoing support (Synapse 2025).
ABC Approach to Behaviour Management
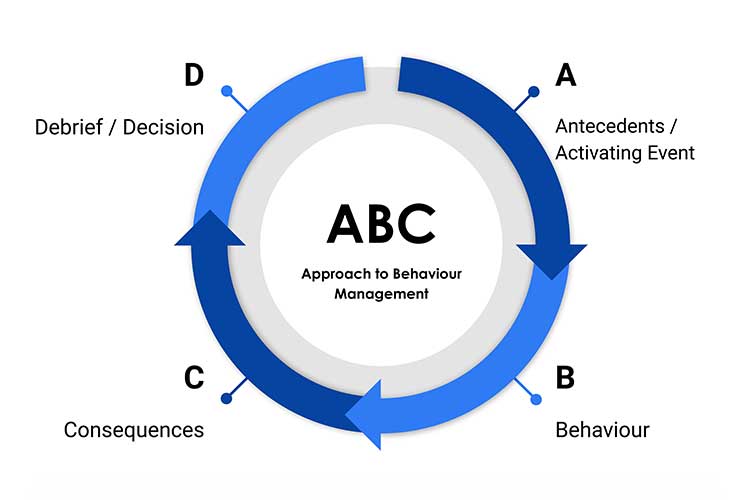
- A: Antecedent / Activating Event - What led to or caused the behaviour?
- B: Behaviour - What is the behaviour?
- C: Consequences - What is the result of the behaviour?
- D: Decide and Debrief - What will be done differently to disrupt the behaviour?
(Dementia Support Australia 2024; Siple 2023)
A: Antecedent or Activating Event
The antecedent or activating event looks at direct or indirect triggers of the behaviour; the why, what, when, where and who.
These stimuli could include:
- Organic causes - e.g. health conditions, pain, fatigue, effects of medications, etc.
- Emotional state - e.g. happiness, anger, etc.
- Cognitions - e.g. what the person may be thinking.
- Environmental factors - e.g. a noisy or unfamiliar environment.
- Social relationships - e.g. interactions with other people.
(ABIOS 2021)
B: Behaviour
The changed behaviour should be defined clearly. Types of BPSD commonly seen include:
- Wandering or absconding
- Depression
- Sundowning
- Anxiety or agitation
- Aggression
- Disruptive or intrusive behaviour
- Hallucinations or delusions
- Socially inappropriate or disinhibited behaviour.
(VIC DoH 2024; NSW Health 2022)
Note, simply labelling the behaviour is not sufficient. You must be able to describe what was observed. For example, did the person yell, cry, punch or use particular words?
C: Consequences
The consequences of the behaviour are the responses from everyone involved. These could include those of the staff, family members or other care recipients who were witnesses to the behaviours.
- Were they emotional and panicked in their response?
- Did they simply ignore the behaviour?
- Did they reprimand the person?
- Were their actions calm and respectful?
(Synapse 2025)
D: Decide and Debrief
The final and additional step to the ABC approach is to decide and debrief. This step allows the care team to come together to consider their findings and collaborate on the best way to manage the situation. Remember that in true person-centred care, the person themself is part of the care team and should be involved in this process, or alternatively, the person’s family or designated decision-makers.
Decisions on what actions to take could involve:
- Using a calm, gentle manner when communicating with the person
- Reducing the number of staff who interact with the person
- Offering more stimulating or distracting activities or exercises
- Stronger, more effective means of communication between staff about potential triggers
- Removing certain stimuli from the environment, such as overly bright lights or loud noises
- Closely monitoring interactions between particular people
- Addressing underlying emotions and referring to other healthcare services when necessary.
(Alzheimer’s Society 2021; VIC DoH 2024)
The ABC Approach in Practice
Scenario: Ted is an 87-year-old resident in a secure aged care facility who is living with dementia. In his younger years, Ted was extremely active and would wake early every morning to walk to the corner milk bar to buy the newspaper.
| Antecedent or Activating Event: | After waking early one morning, Ted attempts to leave through the front entrance of the facility, with the intention of walking to the shops to buy the newspaper. However, he is halted by the locked security door, which requires a keycode to open. |
| Behaviour: | Ted gets agitated and upset when he finds himself locked behind the door. He begins to try to rattle and break the door latch. He is panicked and loudly demands to be let out. |
| Consequences: | The staff member on shift responds to the behaviour in a confrontational manner (‘Hey! Stop that! What are you doing?! You’ll break the door! Go back to bed!’), attempting to stop Ted from waking and disturbing other residents. The staff member forcefully grabs hold of Ted’s wrists in an attempt to stop him from breaking the door lock. The staff member’s response only makes Ted more upset, increasing his distress. His behaviour continues to escalate into yelling and physical aggression. |
| Decide and Debrief: | After the incident, the care team debriefs with Ted’s family and learns about his history, habits and preferences of walking to get the newspaper each morning.
The team also notes that the staff member's response during the shift was inappropriate and recommends that they take a day off from work to de-stress and undergo further communication and de-escalation education. The team decide that the staff member rostered on each morning should now have a newspaper ready to offer Ted when he gets up in the morning, and respectfully offer to walk with him around the facility before returning him back to his room. |
Conclusion
The ABC Approach to behavioural management works best when the person’s behaviour is clearly documented and understood. The first approach should always be non-pharmacological and should involve tweaking the personal and environmental elements that contributed to the event.
The person’s medical prescriber may consider a medication review if the behaviours are ongoing. Many milder behaviours tend to run a course and can resolve in time, and so patience and support are often the best response in these cases (Krishnamoorthy & Anderson 2011).
Note: Always refer to your facility's policy on dealing with difficult or aggressive behaviours. If there is a real risk of danger to you or your clients, security may need to be called.
Test Your Knowledge
Question 1 of 4
Step ‘B’ in the ABC Approach to Behaviour Management refers to…?
Topics
Further your knowledge
 Free
Free Free
Free Free
Free
References
- Acquired Brain Injury Outreach Service 2021, Behaviour Intervention: The ABC of Behaviour, Queensland Government, viewed 28 May 2025, https://www.health.qld.gov.au/__data/assets/pdf_file/0022/384070/abc_behaviour_pro.pdf
- Aged Care Quality and Safety Commission 2025, Draft Strengthened Quality Standards Guidance, Australian Government, viewed 28 May 2025, https://www.health.gov.au/resources/publications/strengthened-aged-care-quality-standards-august-2025?language=en
- Alzheimer’s Society 2021, Reducing and Managing Behaviour That Challenges, Alzheimer’s Society, viewed 29 May 2025, https://www.alzheimers.org.uk/about-dementia/symptoms-and-diagnosis/symptoms/managing-behaviour-changes
- Dementia Support Australia 2024, The ABCDE of Behaviour Support, Dementia Support Australia, viewed 28 May 2025, https://www.dementia.com.au/resource-hub/abcde-of-behaviour-support
- Krishnamoorthy, A & Anderson, D 2011, ‘Managing Challenging Behaviour in Older Adults with Dementia’, Progress in Neurology and Psychiatry, viewed 29 May 2025, https://onlinelibrary.wiley.com/doi/pdf/10.1002/pnp.199
- NSW Health 2022, Assessment and Management of Behaviours and Psychological Symptoms associated with Dementia (BPSD): A Summary Handbook for NSW Health Clinicians Providing Services for People Experiencing BPSD, New South Wales Government, viewed 28 May 2025, https://www.health.nsw.gov.au/mentalhealth/resources/Publications/ass-mgmt-bpsd-summary-handbook-dec-22.pdf
- Siple, A 2023, ‘The ABCD Approach for Managing Neuropsychiatric Symptoms of Dementia’, Nursing, vol. 53, no. 8, viewed 28 May 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10355332/
- Synapse 2025, The ABC Approach to Behaviour Support, Synapse, viewed 28 May 2025, https://synapse.org.au/fact-sheet/the-abc-approach-to-behaviour-support/
- Victoria Department of Health 2024, Managing Dementia, Victoria State Government, viewed 28 May 2025, https://www.health.vic.gov.au/older-people-in-hospital/cognition-dementia-delirium-and-depression/dementia/managing-dementia