Workers employed by National Disability Insurance Scheme (NDIS) providers, who deliver supports to NDIS participants requiring complex bowel care, must be able to provide appropriate care.
This article has been updated in response to the release of Version 3 of the NDIS Practice Standards: High Intensity Support Skills Descriptors (HISSD), which came into effect on 1 February 2023.
What is Complex Bowel Care?
Bowel care is a routine component of personal support (NDIS 2021a).
However, NDIS participants at risk of severe constipation or faecal incontinence may require complex bowel care from support workers with a more specialised skill set (NDIS 2022).
Complex Bowel Care in the NDIS Practice Standards
Complex bowel care is a requirement of the NDIS Practice Standards under the High Intensity Daily Personal Activities Module.
This Practice Standard aims to ensure that NDIS participants requiring complex bowel care receive appropriate support that is relevant and proportionate to their individual needs (NDIS 2021b).
Under these standards, care providers must meet the following quality indicators:
- Participants are enabled to participate in the assessment and development of a complex bowel care plan. This plan identifies possible risks, incidents and emergencies, and what actions need to be taken to manage these situations, including the escalation of care, if necessary. The participant’s health status is reviewed regularly (with the participant’s consent).
- Workers providing complex bowel care are informed by appropriate policies, procedures and training plans.
- Workers providing complex bowel care have received all necessary training from a qualified health practitioner or another appropriately qualified individual.
(NDIS 2021b)
Who Requires Complex Bowel Care?
Complex bowel care may be required for NDIS participants living with:
- Spinal injury or other conditions causing muscle or nerve damage
- Autism
- Stroke
- Neurological conditions
- Cerebral palsy (with a Gross Motor Function Classification System (GMFCS) level of 3, 4 or 5)
- Acquired brain injury.
(NDIS 2022)
A participant who is receiving non-routine treatment such as non-routine pro re nata (PRN) medication for bowel care may also require complex support (NDIS 2022).
Complex Bowel Care Skills Descriptors and Knowledge
The NDIS high intensity support skills descriptors are additional guidance specifically for NDIS workers who are supporting participants with high intensity daily personal activities (HIDPA). Many of these HIDPAs are high-risk and/or intimate care areas that require a high level of care, competency and communication. The high intensity support skills descriptors set out the skills and knowledge required for NDIS workers to effectively and safely support participants with HIDPAs (NDIS 2022).
The high intensity support skills descriptors have been updated as of 1 February 2023 in order to:
- Ensure they reflect contemporary practice and expert advicev
- Align their format and language more closely to the NDIS Workforce Capability Framework.
(NDIS 2023)
Skills Required for Complex Bowel Care
Workers providing complex bowel care under the NDIS should be able to:
- Understand and follow the participant’s support plan
- Ask the participant about their expectations, capacity and preferences for being involved in the delivery of their care
- Ask the participant about their communication preferences, and communicate in their preferred way
- Follow hygiene and infection control principles, including hand hygiene, disinfecting the environment and wearing gloves
- Ensure required equipment and consumables are available and prepared for use
- Provide support in the least intrusive and restrictive way practicable, in alignment with the participant’s daily routine and preferences
- Recognise that bowel health is highly personal for the participant and provide support accordingly
- Support the participant to position themselves for bowel care
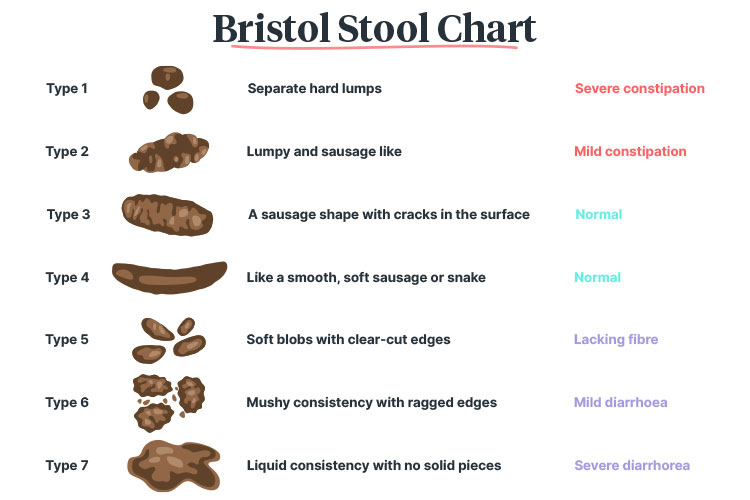
- Use the Bristol Stool Form Scale or other reference guides to observe and record bowel motions, and identify changes that require escalation of care
- Ensure that the participant is clean, comfortable and not experiencing perianal skin irritation
- Identify signs of poor bowel function or other issues and escalate to an appropriate health practitioner immediately
- Work collaboratively with other members of the care team
- Discuss any changes needed to bowel care support with the participant
- Identify, document and report if the participant’s support plan is not meeting their needs
- Support the participant to provide feedback or request changes to their support plan.
(NDIS 2022)
Additionally, workers supporting a participant with a stoma in situ should also be able to:
- Assist the participant in keeping the stoma site healthy and clean
- Repace and dispose of stoma bags
- Monitor and record required information (as indicated by the participant’s support plan), e.g. outputs, hydration and stoma appearance
- Identify issues such as blockages and immediately escalate care to an appropriate health practitioner.
(NDIS 2022)
Knowledge Required for Complex Bowel Care
NDIS Code of Conduct and Practice Standards
Read: The NDIS Practice Standards Explained
The NDIS Practice Standards establish the benchmark of performance, quality and safety that NDIS providers should meet in their delivery of supports and services (NDIS 2021b).
The Standards work alongside the NDIS Code of Conduct to inform NDIS participants about the quality they should be expecting from the supports and services they receive (NDIS 2021b).
The NDIS Code of Conduct sets out expectations for the behaviour of both NDIS workers and participants in order to promote safe and ethical service delivery.
The Importance of Good Bowel Care
Good bowel management is essential for a person’s physical health, self-esteem and overall quality of life (Sober-Williams et al. 2024).
Bowel conditions, particularly faecal incontinence, are highly stigmatised and can have severe social and emotional consequences (Duyos & Ribas 2019). Therefore, good bowel care can help support participants to gain more confidence and lead the life they choose.
Remember that bowel health is a highly personal and embarrassing subject for some people, so participants should always be treated with empathy and dignity.
Communication Supports
Participants may have a variety of communication needs and preferences, such as the use of communication aids or devices, or access to resources in another language (NDIS 2022). Remember to individualise communication to ensure each participant’s needs and preferences are met.
For more information on communication supports, see the following Ausmed resources:
Infection Prevention and Control
It’s essential to be aware of and follow infection control principles, including PPE, handwashing and disinfecting (NDIS 2022).
For more information on infection control, see Ausmed’s Training Module on Infection Prevention and Control.
Scope of Practice
Always work within your scope of practice and your role’s responsibilities. Refer to your manager and/or local policies and procedures for more clarity on your specific role and responsibilities if you are unsure.
Also see Ausmed’s Training Module on Scope of Practice: Care Workers.
Bowel Anatomy and Physiology
When food is consumed, it breaks down in the stomach and passes through the intestines. The walls of the intestines then absorb nutrients from the food. The waste that remains is then passed through the colon and rectum and is excreted (Khan & Chavoustie 2024).
Bowel motions are affected by a variety of factors, such as:
- Diet: Fibre adds bulk to faeces, making it easier to pass, while on the other hand, a low-fibre diet can lead to constipation
- Hydration: Insufficient water intake can lead to constipation
- Probiotics: Consuming probiotics has been found to increase the frequency of bowel movements, decrease bowel transit time and improve the consistency of stools.
(Better Health Channel 2024; Healthy Eating Clinic 2020)
Complex Bowel Conditions
Complex bowel conditions in the NDIS high intensity support skills descriptors include:
- Severe constipation
- Faecal incontinence.
(NDIS 2022)
Constipation
Constipation refers to difficulty defecating over an extended period of time. It is defined as the occurrence of less than three bowel movements per week (Premium Health 2022).
Someone who is constipated may simply have difficulty defecating (with a normal defecation frequency), or they may have a delayed colonic transit time of food from the mouth to the anus, which causes stools to become hard, dry and infrequent (Premium Health 2022).
Common causes of constipation include:
- Insufficient fibre intake
- Insufficient hydration
- Lack of physical activity
- Ignoring the urge to defecate
- Certain medicines
- Stress
- Pregnancy
- Certain conditions, including Parkinson's disease, multiple sclerosis, depression, irritable bowel syndrome and coeliac disease
- Older age.
(Better Health Channel 2024; Healthdirect 2024a)
Signs and symptoms of constipation include:
- Needing to open the bowels less frequently
- Hard, dry stools that might be difficult to pass
- Painfully straining to pass a bowel motion
- Feeling as though there is a blockage preventing a bowel movement
- Having to sit on the toilet for long periods of time
- A sensation that the bowel has not fully emptied after a motion
- Bloated abdomen
- Abdominal cramps.
(Better Health Channel 2024; Mayo Clinic 2023)
Faecal Incontinence
Someone experiencing faecal incontinence has difficulty with bowel control, causing involuntary loss of stools (Healthdirect 2024b).
Common causes of faecal incontinence include:
- Poor toilet habits e.g. straining to pass stools
- Certain medicines
- Weak pelvic floor muscles
- Constipation
- Diarrhoea
- Certain conditions, including Parkinson's disease, multiple sclerosis, depression, diabetes and bowel diseases.
(Healthdirect 2024; Continence Foundation of Australia 2024)
Signs and symptoms of faecal incontinence include:
- Difficulty holding in a bowel movement
- Needing to rush to the toilet to empty the bowels
- Leakage of faeces or flatus.
(Healthdirect 2024)
Autonomic Dysreflexia
Autonomic dysreflexia is a potentially life-threatening complication that can occur in people with spinal cord injury (typically a SCI above T6). It occurs in response to a strong sensory stimulus below the level of the injury, resulting in severe hypertension (ACI 2024).
Autonomic dysreflexia can be triggered by bowel issues such as constipation and faecal impaction. Therefore, good bowel care for participants with SCI is crucial in order to avoid this complication from occurring (ACI 2024).
Signs and symptoms of autonomic dysreflexia include:
- Blood pressure ≥ 20 mmHg above the participant’s baseline systolic level
- Pounding headache, which worsens as BP increases
- Flushed or blotched skin above the level of the SCI
- Pale skin and piloerection (goosebumps) below the level of the SCI
- Dilated pupils and blurry vision
- Chills (with no fever)
- Bradycardia (slow heart rate)
- Shortness of breath
- Feelings of anxiety or apprehension
- Irritability or combative behaviour in people with limited cognition or communication skills.
(ACI 2024)
If you suspect autonomic dysreflexia in a participant you are caring for, you should immediately:
- Alert your manager or an appropriately qualified healthcare practitioner (refer to your organisation’s policies and procedures)
- Elevate the person’s head and lower their legs to reduce blood pressure
- Loosen constrictive clothing
- Monitor blood pressure every 2-5 minutes.
(ACI 2024)
Bowel Care Support
Bowel issues can be managed in a variety of ways, including:
- Enemas
- Laxatives
- Suppositories
- Stool softeners
- Abdominal massage.
(NDIS 2022; Better Health Channel 2014)
Stomas

A stoma is a surgically created artificial opening through which a section or piece of the bowel is brought through the abdomen. This allows waste to be removed from the body directly through the end of the bowel into a collection bag (Healthdirect 2023; Cancer Council Victoria 2021).
There are two types of bowel stoma:
- Colostomy: made from the colon in the large bowel
- Ileostomy: made from the ileum in the small bowel.
(Cancer Council Victoria 2021)
The waste that passes through the stoma is collected in a stoma bag, a pouch made from soft, waterproof material (Clinimed 2024).
This bag fits securely around the stoma and adheres to the abdomen using an attached or detachable flange. The type of bag needed will depend on the type of stoma (CliniMed 2024).
What should a healthy stoma look like?
- The stoma should be pink or red, moist and shiny
- Swelling may be present during the postoperative period but should decrease in size within six to eight weeks
- Minor bleeding may occur in response to trauma but should stop when you apply light pressure to the area
- The border between the stoma and the abdominal skin should be intact, with even, intermittent sutures in situ
- The skin surrounding the stoma should be intact, healthy and look similar to the skin on the other side of the abdomen
- The stoma should be protruding between 2 to 3 cm from the skin.
(WACHS 2025)
How to care for skin around the stoma:
- Use warm water and a soft, disposable cloth to clean the skin
- Try to avoid using soap, as this can impair adhesion - if you do need soap, use a mild product that won’t leave residue behind
- Dry the skin using a soft, disposable cloth
- Avoid using:
- Soaps containing lotions
- Skin care creams and lotions
- Powders
- Wipes
- Isopropyl alcohol
- Steroidal ointments and medications.
(WACHS 2025; Dansac 2018)
Issues at the stoma site:
The following signs and symptoms require escalation of care to an appropriately qualified medical practitioner:
- Pale, dark, dusky or black stoma
- Excessive swelling
- Abnormal bleeding
- Disruption to the mucocutaneous junction
- Dehiscence
- Extruding serosal tissue
- Skin redness, erythema, rashes or irritation
- Impaired skin integrity
- Skin pain or tenderness
- Retracted stoma (where the stoma slides back into the abdomen below skin level)
- Prolapsed stoma (where the stoma slides out of the abdomen and protrudes more than 5 cm from skin level)
- Infection
- Parastomal hernia (wherein part of the bowel protrudes through the stoma)
- Diarrhoea
- Dehydration
- Narrowing of the stoma
- Difficulty passing stools through the stoma
- Obstruction of the stoma due to scar tissue
- Impacted faeces
- Kidney stones
- Gallstones
- Necrosis
- Decreased output
- Excessive output
- Incorrectly fitted stoma appliance
- Appliance leakage.
(WACHS 2025; CHS 2023; Finlay et al. 2018; Better Health Channel 2011)
For more information on stomas and stoma care, see the Ausmed Course Acute Stoma Care.
Management
You may have specific documentation and reporting responsibilities, such as handover, observations and incident reporting (NDIS 2022). Refer to your organisation’s policies and procedures for further information on what is required.
You should also be aware of the process for requesting a review of a participant’s care (NDIS 2022). Refer to your organisation’s policies and procedures for further information.
When to Escalate Care
The participant should be referred to a health practitioner if they are experiencing the following complications:
- Overflow
- Bowel obstruction
- Perforation
- Faecal impaction
- Strangulated hernia
- Infection
- Autonomic dysreflexia
- Undiagnosed rectal bleeding
- Undiagnosed diarrhoea
- Poor nutrition or hydration.
(RCN 2019; NDIS 2021a)
Conclusion
Remember that bowel health may be embarrassing and highly personal for some people. Therefore, it is essential to communicate with participants empathetically.
Test Your Knowledge
Question 1 of 3
Which one of the following conditions may require complex bowel care under the NDIS?
Topics
Further your knowledge
References
- Agency for Clinical Innovation 2024, Treatment of Autonomic Dysreflexia for Adults and Adolescents with Spinal Cord Injuries, New South Wales Government, viewed 12 February 2025, https://aci.health.nsw.gov.au/__data/assets/pdf_file/0007/155149/ACI-Treatment-of-autonomic-dysreflexia-for-adults-and-adolescents-with-spinal-cord-injuries.pdf
- Better Health Channel 2024, Constipation, Victoria State Government, viewed 12 February 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/constipation
- Better Health Channel 2011, Stoma After Ileostomy or Colostomy, Victoria State Government, viewed 12 February 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/stoma-after-ileostomy-or-colostomy
- Canberra Health Services 2023, Procedure: Stoma Management – Adults, Adolescents, Children, Infants and Neonates, ACT Government, viewed 12 February 2025, https://www.canberrahealthservices.act.gov.au/about-us/policies-and-guidelines
- Cancer Council Victoria 2021, Having a Stoma, Cancer Council Victoria, viewed 12 February 2025, https://www.cancervic.org.au/cancer-information/types-of-cancer/bowel_cancer/having-a-stoma.html
- CliniMed 2024, What is a Stoma Bag?, CliniMed, viewed 11 February 2025, https://www.clinimed.co.uk/stoma-care/stoma-types
- Continence Foundation of Australia 2024, Faecal Incontinence, Continence Foundation of Australia, viewed 12 February 2025, https://www.continence.org.au/types-incontinence/faecal-incontinence
- Dansac 2018, Caring for the Skin Around Your Stoma, Dansac, viewed 12 February 2025, https://www.dansac.com.au/en-au/livingwithastoma/healthyskinaroundyourstoma/caringfortheskinaroundyourstoma
- Duyos, AM & Ribas, Y 2019, ‘Quality of Life Considerations on Fecal Incontinence’, Current Topics in Faecal Incontinence, viewed 12 February 2025, https://www.intechopen.com/books/current-topics-in-faecal-incontinence/quality-of-life-considerations-on-fecal-incontinence
- Finlay, B Sexton, H & McDonald, C 2018, ‘Care of Patients With Stomas in General Practice’, Australian Journal of General Practice, vol. 47, no. 6, viewed 12 February 2025, https://www1.racgp.org.au/ajgp/2018/june/stomas-in-gp
- Healthdirect 2023, Living with a Stoma, Australian Government, viewed 12 February 2025, https://www.healthdirect.gov.au/living-with-a-stoma
- Healthdirect 2024a, Constipation, Australian Government, viewed 12 February 2025, https://www.healthdirect.gov.au/constipation
- Healthdirect 2024b, Faecal Incontinence, Australian Government, viewed 12 February 2025, https://www.healthdirect.gov.au/faecal-incontinence
- The Healthy Eating Clinic 2020, Probiotics and Your Poo, The Healthy Eating Clinic, viewed 12 February 2025, https://healthyeatingclinic.com.au/probiotics-and-your-poo/
- Khan, A & Chavoustie, CT 2024, ‘What is Fecal Impaction (Impacted Bowel) and How Is It Treated?’, Healthline, 19 January, viewed 12 February 2025, https://www.healthline.com/health/fecal-impaction
- Mayo Clinic 2023, Constipation, Mayo Clinic, viewed 12 February 2025, https://www.mayoclinic.org/diseases-conditions/constipation/symptoms-causes/syc-20354253
- NDIS Quality and Safeguards Commission 2021a, DIS Practice Standards: Skills Descriptors, Australian Government, viewed 12 February 2025, https://www.ndiscommission.gov.au/sites/default/files/2022-02/fact-sheetndis-practice-standardshigh-intensity-skills-descriptors.pdf
- NDIS Quality and Safeguards Commission 2021b, NDIS Practice Standards: NDIS Practice Standards and Quality Indicators, Australian Government, viewed 12 February 2025, https://www.ndiscommission.gov.au/sites/default/files/2022-02/ndis-practice-standards-and-quality-indicatorsfinal1_1.pdf
- NDIS Quality and Safeguards Commission 2022, NDIS Practice Standards: High Intensity Support Skills Descriptors, Australian Government, viewed 12 February 2025, https://www.ndiscommission.gov.au/sites/default/files/2024-09/High%20Intensity%20support%20skills%20descriptors.pdf
- Premium Health 2022, Bowel Management - Elimination, Premium Health, viewed 12 February 2025, https://premiumhealth.com.au/resources/bowel-management-elimination-booklet
- Royal College of Nursing 2019, Bowel Care, Royal College of Nursing, viewed 12 February 2025, https://www.berkshirehealthcare.nhs.uk/media/110205484/bowel-care-rcn-guide.pdf
- Sober-Williams, EK, Lee, RHY, Whitehurst, DGT et al. 2024, ‘Bowel Burdens: A Systematic Review and Meta-Analysis Examining the Relationships Between Bowel Dysfunction and Quality of Life After Spinal Cord Injury’, Spinal Cord, vol. 62, viewed 12 February 2025, https://www.nature.com/articles/s41393-024-01002-8


