Diabetic retinopathy is the most common cause of vision loss in Western working-age adults (Shukla & Tripathy 2023). In fact, among the 1.7 million Australians who have diabetes, about one-third are estimated to have some degree of diabetic retinopathy (CERA 2025).
What is Diabetic Retinopathy?
Diabetic retinopathy is a microvascular disorder caused by long-term diabetes, characterised by gradual vision-threatening damage to the retinal blood vessels (Shukla & Tripathy 2023).
If left untreated, diabetic retinopathy can result in irreversible blindness (Shukla & Tripathy 2023).
What Causes Diabetic Retinopathy?
Diabetic retinopathy is associated with chronic hyperglycaemia and occurs when excess glucose obstructs the blood vessels in the retina, cutting off their blood supply (Shukla & Tripathy 2023; Mayo Clinic 2023).
There are two stages of diabetic retinopathy:
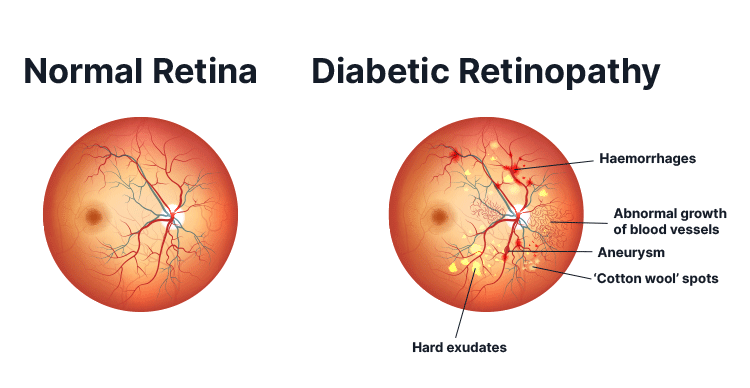
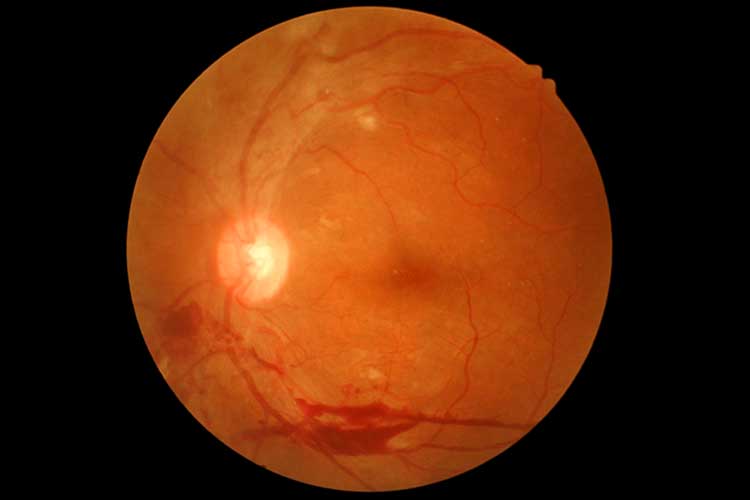
- Non-proliferative diabetic retinopathy is the initial stage of the condition and is characterised by the weakening of the retinal blood vessels. This causes the blood vessels to thin and bulge outwards, and consequently, they may leak fluid and bleed into the retina.
- Proliferative diabetic retinopathy is the more advanced, serious stage of diabetic retinopathy. It occurs when new, abnormal blood vessels begin to grow in response to the reduced blood supply to the existing blood vessels. These new blood vessels are very fragile and may leak into the vitreous humour. This can cause the formation of scar tissue that may pull on the retina and lead to retinal detachment.
(myDr 2024; Mayo Clinic 2023)
Macular oedema, wherein fluid leakage from the retinal blood vessels causes swelling of the macula, can occur in any stage of diabetic retinopathy. This may impair central vision, which is used for tasks such as reading and driving (Better Health Channel 2015; myDr 2024). Macular oedema is the most common cause of vision loss in diabetes (Kohli et al. 2024).
Risk Factors for Diabetic Retinopathy
All people with type 1 and 2 diabetes are at risk of diabetic retinopathy. However, effectively controlling diabetes reduces the likelihood (Vision Initiative 2023).
As a general rule, the longer the patient has had diabetes, the greater the risk of developing diabetic retinopathy (CERA 2025).
Factors that might increase the risk of diabetic retinopathy include:
- Having diabetes for longer than 10 years
- Going through puberty
- Pregnancy (due to increases in hormones)
- Hypertension
- Obesity
- Dyslipidaemia (lipid imbalance)
- Poor diabetes management
- Nephropathy (diabetic kidney disease)
- Genetic factors
- Increased inflammatory factors
- Apolipoprotein (a plasma protein)
- Hormones (leptin and adiponectin)
- Vitamin D deficiency
- Oxidative stress
- Being of Aboriginal or Torres Strait Islander descent.
(myDr 2024; Shukla & Tripathy 2023)
Symptoms of Diabetic Retinopathy

There are typically no symptoms in the early stages of diabetic retinopathy (CERA 2025). In advanced stages, patients might experience:
- Blurry, distorted or patchy vision that can’t be corrected with prescription lenses
- Eye floaters (specks that appear to move across the field of vision), which may have a red or brown tinge
- A smudge in the vision of one eye
- Difficulty reading, watching television or recognising faces
- Pain in one or both eyes
- Difficulty seeing straight lines (may appear bent or wavy)
- Sensitivity to glare
- Difficulty seeing at night
- Balance issues.
(Healthdirect 2024; CERA 2025; Vision Initiative 2023)
Complications of Diabetic Retinopathy
Potential complications of diabetic retinopathy include:
- Vitreous haemorrhage, which can temporarily fill the vitreous cavity and block vision Retinal detachment, which can result in severe vision loss
- Glaucoma
- Blindness.
(Mayo Clinic 2023)
Diagnosing Diabetic Retinopathy
Regular eye examinations, early diagnosis and treatment are essential to preventing severe vision loss. This includes a baseline eye examination when diabetes is first diagnosed (Better Health Channel 2015).
Diabetic retinopathy is diagnosed through an eye examination that typically comprises digital retinal photography and a dilated eye exam. In this exam, eye drops are used to dilate the eyes so that the practitioner can get a better view of the eye using a slit lamp or ophthalmoscope to examine for evidence of diabetic retinopathy (CERA 2025; myDr 2024).
Treatment for Diabetic Retinopathy
Diabetic retinopathy can’t be cured, but if detected early, management strategies can prevent vision loss before any damage is done. If the patient has already experienced vision loss due to diabetic retinopathy, treatment can stop it from worsening but may be unable to restore vision that has been lost (Diabetes Australia 2024; myDr 2024).
The best way to prevent vision loss is the effective management of diabetes, including:
- Regular eye examinations
- Maintaining a healthy lifestyle
- Maintaining a healthy and balanced diet
- Regular physical activity
- Managing blood pressure and cholesterol.
(Dirani et al. 2013)
Treatment is typically indicated when diabetic retinopathy is in a proliferative stage or macular oedema is present. It might involve one or more of the following:
- Retinal laser treatment to help prevent further vision loss and reduce the risk of worsening
- Intravitreal injection, which involves injecting medicine (either a vascular endothelial growth factor inhibitor or steroid) directly into the vitreous - injections may be required regularly
- Vitrectomy (surgical removal of the vitreous).
(CERA 2025; Dirani et al. 2013)
Preventing Diabetic Retinopathy
The best way to prevent vision loss from diabetic retinopathy is for all people with diabetes to undergo regular eye examinations, as damage can usually be avoided if diabetic retinopathy is detected early enough (CERA 2025).
It’s essential that people with diabetes undergo an eye examination:
- When they are first diagnosed with diabetes, and
- Every two years thereafter (annually for Aboriginal or Torres Strait Islander people), and
- Immediately, if they notice any changes in their vision.
(Vision Initiative 2023)
In order to increase the number of people with diabetes undergoing regular eye checks, Diabetes Australia and Vision 2020 Australia have established an eye check reminder program called KeepSight.
For more information, see KeepSight’s website.
Test Your Knowledge
Question 1 of 3
As a general rule, how often should people with diabetes undergo eye checks?
Topics
Further your knowledge
References
- Better Health Channel 2015, Diabetic Retinopathy, Victoria State Government, viewed 23 May 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/diabetic-retinopathy
- Centre for Eye Research Australia 2025, Diabetic Eye Disease, CERA, viewed 23 May 2025, https://www.cera.org.au/conditions/diabetic-eye-disease/
- Diabetes Australia 2024, Your Eye Health and Diabetes, Diabetes Australia, viewed 23 May 2025, https://www.diabetesaustralia.com.au/living-with-diabetes/preventing-complications/eye-health/
- Dirani, M, Shaw, J & Crowston, J 2013, Out of Sight: A Report Into Diabetic Eye Disease in Australia, Baker IDI Heart and Diabetes Institute and Centre for Eye Research Australia, viewed 23 May 2025, https://baker.edu.au/-/media/documents/impact/outofsightreport.pdf?la=en
- Healthdirect 2024, Diabetic Retinopathy, Australian Government, viewed 23 May 2025, https://www.healthdirect.gov.au/diabetic-retinopathy
- Kohli, P, Tripathy, K & Patel, BC 2024, ‘Macular Edema’, StatPearls, viewed 23 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK576396/
- Mayo Clinic 2023, Diabetic Retinopathy, Mayo Clinic, viewed 23 May 2025, https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
- myDr 2024, Retinopathy in Diabetes, myDr, viewed 23 May 2025, https://www.mydr.com.au/retinopathy-in-diabetes/
- Shukla, UV & Tripathy, K 2023, ‘Diabetic Retinopathy’, StatPearls, viewed 23 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK560805/
- Vision Initiative 2023, Diabetic Retinopathy, Vision Initiative, viewed 23 May 2025, https://www.visioninitiative.org.au/common-eye-conditions/diabetic-retinopathy