Dysphagia is a common condition seen in many long-term care clients, with chewing and swallowing problems affecting between 30 and 50% of Australian aged care residents (Erickson 2019).
What is Dysphagia?

Dysphagia is difficulty swallowing. This can include having problems with:
- Sucking
- Swallowing
- Drinking
- Chewing
- Eating
- Dribbling saliva
- Keeping the lips closed.
(Healthdirect 2022)
Dysphagia can make swallowing painful and in some cases, impossible. People with dysphagia may experience gagging, coughing or choking when eating and drinking (Mayo Clinic 2023).
Note: While dysphagia sounds similar to dysphasia, these two terms refer to separate conditions. While dysphagia refers to difficulty swallowing, dysphasia (also known as aphasia) refers to difficulty speaking. Even though these are two different conditions, they both commonly affect people who have had a neurological event such as a stroke and are both treated by speech pathologists (Brouhard et al. 2023).
Dysphagia Under the Strengthened Aged Care Quality Standards
Standard 5: Clinical Care - Outcome 5.5: Clinical Safety (Action 5.5.2) under the strengthened Aged Care Quality Standards requires aged care organisations to establish processes for ensuring safe chewing and swallowing during:
- Eating
- Drinking
- Talking
- Oral medication administration
- Oral care.
(ACQSC 2024a)
Causes and Risk Factors for Dysphagia
Dysphagia is not necessarily part of the normal ageing process (Health.vic 2015). However, it is not uncommon for older adults to experience presbyphagia - age-related changes to the swallowing mechanism (Thiyagalingam et al. 2021).
Presbyphagia can include:
- Reduced strength of the muscles for mastication (chewing)
- Weak lip seal, causing clients to drool or lose food anteriorly from their mouth
- Reduced tongue strength, which can impact the ability to safely form a bolus
- Delayed swallow reflex, which can cause foods or fluids to enter the pharynx and airway too soon
- Impaired airway closure and airway protection, increasing the risk of aspiration (food and fluids entering the lungs) and choking
- Reduced food bolus transfer through the mouth and pharynx, causing foods and fluids to collect in the mouth or pharynx
- Decreased flexibility of the upper oesophageal sphincter
- Delayed oesophageal emptying
- Weak or missing teeth
- Dryer mucosal surfaces in the mouth and throat.
(Thiyagalingam et al. 2021; Nestle Health Science 2018)
While presbyphagia can be a predisposing factor to dysphagia, an older adult’s swallow is not inherently an issue (Thiyagalingam et al. 2021; MSAC 2018). Instead, dysphagia is most commonly associated with underlying conditions that have a greater prevalence in older populations (Smithard et al. 2016) and interrupt the swallowing process, such as:
- Stroke (about 50% of stroke survivors)
- Dementia (about 84% of people living with dementia)
- Head injury
- Alzheimer's disease
- Neurodegenerative conditions such as Parkinson’s disease, motor neurone disease (MND) and multiple sclerosis
- Cerebral palsy
- Achalasia
- Muscle issues affecting the face or neck or spasms affecting the oesophagus
- Structural problems such as cancers of the oesophagus
- Head and neck cancers requiring radiotherapy or surgical treatment
- Reflux
- Age-related changes
- Frailty.
(Erickson 2019; Healthdirect 2022; Thiyagalingam et al. 2021
Types of Dysphagia
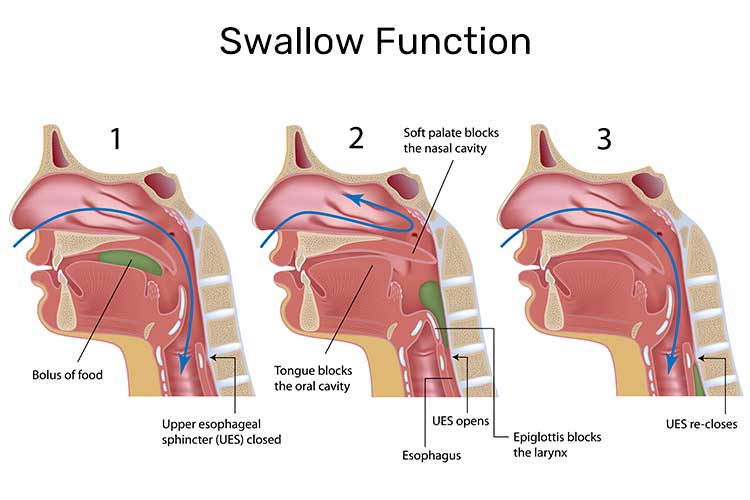
The swallowing process is broken down into three stages:
- Oral
- Pharyngeal
- Oesophageal
Dysphagia can affect just one of these phases or a combination of all three. Because of the nature of the swallowing process, oral and pharyngeal dysphagia are often grouped together - this is known as oropharyngeal dysphagia.
Oropharyngeal dysphagia causes difficulty moving food and fluids around the mouth, forming a bolus (the chewed-up mass of food to be swallowed) and ‘initiating a swallow’. This type of dysphagia is commonly associated with stroke, dementia and Parkinson’s disease (Health.vic 2015; Nestle Health Science 2018).
Signs and Symptoms of Dysphagia
Signs and symptoms of dysphagia can include:
- Inability to swallow
- Pain when swallowing
- Food feeling stuck in the throat, inducing coughing
- Food going down the wrong way
- Drooling
- Hoarseness of the voice
- Regurgitation
- Persistent heartburn
- Weight loss
- Coughing or gagging when swallowing
- Frequent throat clearing during or after eating and drinking
- Shortness of breath when eating and drinking
- Taking a long time to finish meals (more than 30 minutes)
- Frequent chest infections with no known cause.
(Mayo Clinic 2023; Speech Pathology Australia 2024)
Assessing Dysphagia
Clients displaying the above symptoms may require referral to a speech pathologist, who will assess and provide interventions for the swallowing difficulty. This may include recommending food texture and drink thickness modifications to manage the risk of eating and drinking, and teaching swallow rehabilitation exercises and safe swallowing strategies. Speech pathologists can also conduct videofluoroscopy (VFSS) and fiberoptic endoscopic evaluation of swallowing (FEES) to assess swallow safety. In severe cases, the client might require enteral feeding (Speech Pathology Australia 2024).
Risks Associated With Dysphagia
Dysphagia can cause aspiration - where food, liquid or saliva tracks into or is inhaled into the lungs rather than being ingested into the stomach (Health.vic 2015).
This, in turn, can lead to aspiration pneumonia, an extremely serious and potentially fatal complication. Aspiration pneumonia is the most common cause of death in people with dysphagia (Health.vic 2015).
Factors that can increase the risk of developing aspiration pneumonia are:
- Older age
- Nasogastric tube in-situ
- Poor oral care/hygiene
- Poor cough reflex.
(Sanivarapu et al. 2024)
Dysphagia can also cause choking, which is the second most common cause of preventable death in aged care facilities (Erickson 2019).
Furthermore, people with dysphagia are at increased risk of developing malnutrition or dehydration if they cannot consume adequate amounts of food and fluid due to their condition (Healthdirect 2022).
The IDDSI Framework For Food Texture and Drink Thickness
Note: This Article is NOT an official IDDSI resource and is NOT meant to replace materials and resources on https://iddsi.org/. For the most current information and resources, see https://iddsi.org/.
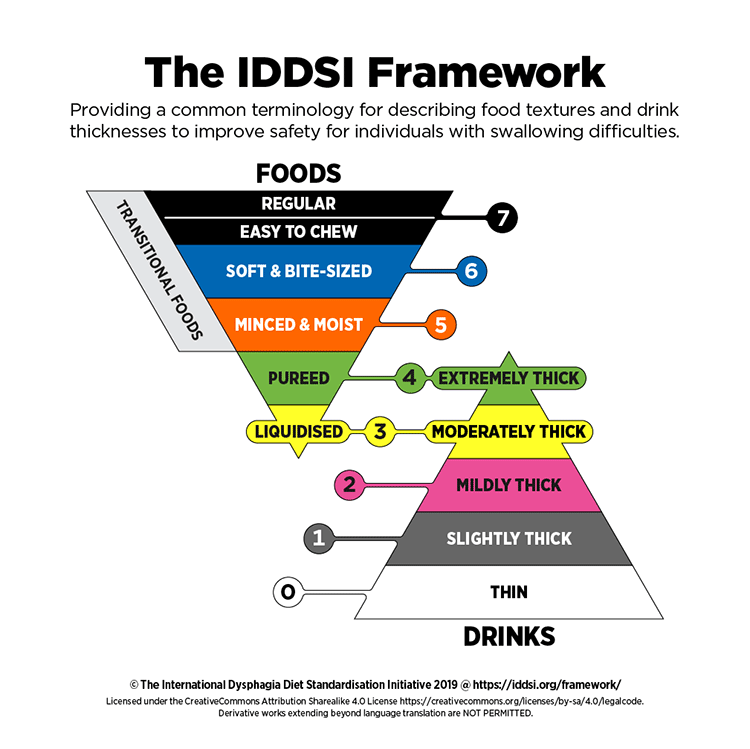
The International Dysphagia Diet Standardisation Initiative (IDDSI) is the global standard of texture modification for people with dysphagia, regardless of age or care setting (IDDSI 2020).
Liquid Consistency
Depending on a client’s swallow test (usually performed by a speech pathologist), they will be prescribed a particular consistency of liquid to match their ability.
Liquid consistency can be anywhere from puree-thick, to runny and thin.
Standards for Texture Modified Fluid Consistency
- Level 0 - Thin
- Level 1 - Slightly thick
- Level 2 - Mildly thick
- Level 3 - Moderately thick
- Level 4 - Extremely thick.
(IDDSI 2020)
Some of these fluids will come pre-prepared to the desired consistency, but others may need to have fluid thickener added to achieve the correct consistency for your client.
Food Consistency
Like liquids, foods should be served at a manageable consistency as well, depending on the client’s ability to chew or swallow.
Standards for Texture Modified Food Consistency
- Level 3 - Liquidised
- Level 4 - Pureed
- Level 5 - Minced and moist
- Level 6 - Soft and bite-sized
- Level 7 - Easy to chew/regular.
(IDDSI 2020)
Some people will be on normal consistency foods and can eat anything that they choose, while others may be at the stage of consuming slightly thickened liquids in addition to normal consistency food.
Brief Diet Descriptors
Easy to chew - IDDSI level 7:
- Doesn’t include hard, tough, chewy, fibrous, stringy, crunchy or crumbly bits, pips, seeds, fibrous parts of fruit, husks or bones
- The person must be able to bite, chew and orally processes soft foods for long enough to form a bolus that is ready to swallow
- Teeth are not necessarily required
- The person must be able to chew and orally process soft foods without becoming tired easily
- Food pieces can be any size - therefore, there is a choking risk for those with a clinically identified increased risk of choking.
Soft and bite-sized - IDDSI level 6:
- Biting is not required
- Chewing is required
- Food piece sizes are designed to minimise choking risk and must be no longer than 1.5 cm cubed.
Minced and moist - IDDSI level 5:

- Biting is not required
- Minimal chewing is required
- Soft small particles must be able to be separated by tongue force alone
- Food piece sizes are designed to minimise choking risk and must be no longer than 15 mm in length and 4 mm in width.
Pureed - IDDSI level 4:
- Usually eaten with a spoon (although a fork is possible)
- Cannot be sucked through a straw
- Does not require chewing.
(IDDSI 2019)
For all diet description information, please visit: Complete IDDSI Framework
Texture Modification Under the Strengthened Aged Care Quality Standards
Standard 6: Food and Nutrition - Outcome 6.3: Provision of food and drink (Action 6.3.1) requires that menus in residential aged care organisations (including those for texture-modified diets):
- Are developed alongside older people, chefs/cooks and an Accredited Practising Dietitian
- Are routinely varied and provide older people with the opportunity to choose what they eat and drink
- Allow older people to meet nutritional requirements
- Are reviewed at least once every year by an Accredited Practising Dietitian.
(ACQSC 2024b)
Furthermore, according to Action 6.3.3, all meals, drinks and snacks provided by residential aged care facilities (including those prepared for residents with specific dietary needs) should:
- Be appetising and tasty
- Be served at an appropriate temperature and look visually appealing - this includes texture-modified foods, which can be enhanced using tools like moulds
- Be prepared and served safely
- Meet older people’s individually assessed needs
- Align with older people’s preferences
- Match the menu.
(ACQSC 2024b)
Caring for Clients with Dysphagia
Nutrition and Hydration
Dysphagia can make eating slow, difficult, and tiring. This reduces the amount and variety of foods and drinks a person can consume, which in turn can make it difficult to maintain adequate nutrition and hydration (Mayo Clinic 2023).
While texture-modified foods and drinks are easier and safer for people with dysphagia to consume, they can cause unappealing changes to appearance, flavour and mouthfeel. Therefore, some clients may refuse or hesitate to consume them, which further increases the risk of malnutrition and dehydration (ACQSC 2023).
Using moulds - for example, forming carrot puree into the shape of a carrot using a mould - may help make texture-modified food more palatable and easier to identify than a nondescript coloured blob. Another strategy to make texture-modified foods more appetising is to use flavoured foams and dusts (e.g. bacon dust) (Egan 2019).
Medications
People with dysphagia can often find it difficult to swallow tablets and capsules. Due to a lack of availability of other forms of medicine such as oral liquids, patches and suppositories, medication crushing is common in aged care facilities. However, altering the form of a solid medicine is a ‘significant source of medication error and harm to patients’ and can lead to adverse outcomes such as increased toxicity, reduced efficacy and instability of the medicine (Taylor & Glass 2018).
Therefore, medication crushing must only take place after referring to the medicine’s guidelines, references and/or product information (Taylor & Glass 2018).
Consider the following alternative options instead:
- Stopping unnecessary medicines
- Seeking the medicine in a different commercially available dosage form
- Checking to see if another medicine in the same dosage class is available in a different dosage form
- Using extemporaneously compounded medicines
- Using medication lubricants
- Consulting with the client’s speech pathologist to improve swallowing function
(Taylor & Glass 2018)
Oral Hygiene
Good oral hygiene is especially important in older adults with dysphagia. This is because the mouth contains pathogens. If unclean saliva is aspirated, the risk of developing serious aspiration pneumonia increases. Extra care needs to be taken to remove the build-up of food, drink, and bacteria from the mouth (Hanrahan Health 2021).
General Tips
- Minimise background noise and distractions during meals
- Supervise meals if necessary
- Ensure the client is seated upright and well-supported during meals
- Encourage the client to eat slowly, one bite at a time, and ensure each bite has been swallowed before they take another
- Prompt the client to cough between swallows to clear their throat
- Follow any specific instructions given by the client’s health professionals, such as head positioning or using special utensils
- If the client struggles significantly during the meal, pause and consult their speech pathologist or general practitioner
- Have the client remain sitting upright for at least 30 minutes after each meal
- Maintain good oral hygiene by ensuring the client’s mouth is clear of food after meals and ensuring their teeth are brushed regularly
- Consider using specialised adaptive equipment to enhance safety and independence
(ABIOS 2021)
When to Escalate Care
The following signs and symptoms require an escalation of care:
- Wet, gurgly voice when eating or drinking
- Coughing when eating or drinking
- Difficult, rapid or shallow breathing after eating or drinking
(NHS 2023)
Test Your Knowledge
Question 1 of 3
Which of the following is NOT a common symptom of dysphagia?
Topics
Further your knowledge

 Free
Free Free
Free Free
Free Free
Free
 Free
Free



References
- Aged Care Quality and Safety Commission 2024a, Standard 5: Clinical Care, Australian Government, viewed 20 June 2024, https://www.health.gov.au/resources/publications/strengthened-aged-care-quality-standards-august-2025?language=en
- Aged Care Quality and Safety Commission 2024b, Standard 6: Food and Nutrition, Australian Government, viewed 20 June 2024, https://www.health.gov.au/resources/publications/strengthened-aged-care-quality-standards-august-2025?language=en/food-and-nutrition
- Aged Care Quality and Safety Commission 2023, Nutrition and Texture Modified Food and Drink, Australian Government, viewed 20 June 2024, https://www.agedcarequality.gov.au/sites/default/files/media/fnd_workers_texturemodified.pdf
- Acquired Brain Injury Outreach Service 2021, Top Tips to Help Someone with a Swallowing Difficulty, Queensland Government, viewed 20 June 2024, https://www.health.qld.gov.au/__data/assets/pdf_file/0022/674041/dyphagia_toptips_fsw.pdf
- Brouhard, R, Hazan, JH & Underwood, A 2023, ‘Dysphagia vs Dysphasia’, Verywell Health, 5 September, viewed 20 June 2024, https://www.verywellhealth.com/first-aid-phraseology-dysphagia-vs-dysphasia-1298200
- Egan, C 2019, ‘ ‘We Eat with our Eyes’: Getting Food Right in Aged Care’, HelloCare, viewed 20 June 2024, https://hellocare.com.au/eat-eyes-getting-food-right-aged-care/
- Erickson, E 2019, ‘Dysphagia - A Difficult Diagnosis to Swallow’, Aged Care Guide, 12 March, viewed 20 June 2024, https://www.agedcareguide.com.au/talking-aged-care/dysphagia-a-difficult-diagnosis-to-swallow
- Hanrahan Health 2021, Oral Health and Dysphagia, Hanrahan Health, viewed 20 June 2024, https://www.hanrahanhealth.com.au/blog/oral-health-and-dysphagia
- Healthdirect 2022, Dysphagia (Difficulty Swallowing), Australian Government, viewed 20 June 2024, https://www.healthdirect.gov.au/dysphagia
- Health.vic 2015, Swallowing Process and its Impact on Health, Victoria State Government, viewed 20 June 2024, https://www.health.vic.gov.au/patient-care/swallowing-process-and-its-impact-on-health
- International Dysphagia Diet Standardisation Initiative 2019, Complete IDDSI Framework Detailed Definitions 2.0|2019, IDDSI, viewed 20 June 2024, https://iddsi.org/IDDSI/media/images/Complete_IDDSI_Framework_Final_31July2019.pdf
- International Dysphagia Diet Standardisation Initiative 2020, What is IDDSI?, IDDSI, viewed 20 June 2024, https://iddsi.org/IDDSI/media/images/Posters/IDDSI_Poster_What_is_IDDSI_Jan2020.pdf
- Mayo Clinic 2023, Dysphagia, Mayo Clinic, viewed 20 June 2024, https://www.mayoclinic.org/diseases-conditions/dysphagia/symptoms-causes/syc-20372028
- Melbourne Swallow Analysis Centre 2018, Presbyphagia/ or Swallowing and Ageing, MSAC, viewed 20 June 2024, https://www.melbswallow.com.au/resources/presbyphagia-or-swallowing-and-ageing/
- National Health Service 2023, Dysphagia (Swallowing Problems), NHS, viewed 20 June 2024, https://www.nhs.uk/conditions/swallowing-problems-dysphagia/
- Nestle Health Science 2018, ‘Dysphagia and Nutritional Considerations’, HelloCare, 19 August, viewed 20 June 2024, https://hellocare.com.au/dysphagia-nutritional-considerations/
- Sanivarapu, RR, Vaqar, S & Gibson, J 2024, ‘Aspiration Pneumonia’, StatPearls, viewed 20 June 2024, https://www.ncbi.nlm.nih.gov/books/NBK470459/
- Smithard et al. 2016, ‘Dysphagia: A Geriatric Giant?’, Medical and Clinical Reviews, vol. 2, viewed 20 June 2024, https://www.researchgate.net/publication/310834419_Dysphagia_A_Geriatric_Giant
- Speech Pathology Australia 2024, Swallowing, Speech Pathology Australia, viewed 20 June 2024, https://www.speechpathologyaustralia.org.au/SPAweb/Resources_for_the_Public/Fact_Sheets/Fact_Sheets.aspx
- Taylor, S & Glass, B 2018, ‘Altering Dosage Forms for Older Adults’, Australian Prescriber, vol. 41, no. 6, viewed 20 June 2024, https://www.nps.org.au/australian-prescriber/articles/altering-dosage-forms-for-older-adults
- Thiyagalingam, S, Kulinski, AE & Thorsteinsdottir, B, Shindelar, KL & Takahashi, PY 2021, ‘Dysphagia in Older Adults’, Thematic Review on Aging, vol. 96, no. 2, viewed 20 June 2024, https://www.mayoclinicproceedings.org/article/S0025-6196(20)30902-2/fulltext