Healthcare workers are responsible for protecting their patients’ health and safety. This includes preventing the transmission of bloodborne viruses, particularly when performing exposure prone procedures (EPPs).
All registered health practitioners who perform EPPs now have to declare that they comply with the Communicable Diseases Network Australia’s Australian National Guidelines for the Management of Healthcare Workers Living with Blood Borne Viruses and Healthcare Workers Who Perform Exposure Prone Procedures at Risk of Exposure to Blood Borne Viruses, including any testing requirements (NMBA 2021).
This commitment must be made upon initial registration. At each renewal, the practitioner must state that they did comply with the CDNA guidelines in the previous registration period and will commit to complying again in the next registration period (NMBA 2021).
What are Exposure Prone Procedures?
Exposure prone procedures (EPPs) are medical processes where there is potential for the healthcare worker to become injured and bleed into a patient’s open tissues (CDNA 2019).
EPPs involve the HCW’s hands (gloved or ungloved) making contact with sharp instruments, needle tips or sharp tissues such as teeth inside a patient’s open body cavity, wound or confined anatomical space where the HCW’s hands or fingertips are not completely visible throughout the procedure (CDNA 2017).
EPPs include certain types of:
- Cardiothoracic surgery
- Dentistry
- Gynaecological surgery
- Neurosurgery
- Obstetric/midwifery procedures
- Open surgical procedures
- Orthopaedic procedures
- Otolaryngology, head and neck surgery
- Cosmetic surgery
- Trauma.
(CDNA 2019)
A more extensive list of examples can be found in Guidance on Classification of Exposure Prone and Non-exposure Prone Procedures in Australia 2017..

Procedures that are not considered EPPs are those where:
- The HCW’s hands are visible and outside of the patient’s body at all times, or
- There is no potential for the HCW’s hands to be injured by sharp instruments or tissue.
(CDNA 2017)
Note that some non-EPP procedures may escalate and will require a professional who is appropriately qualified to perform EPPs (CDNA 2017).
The major risk associated with EPPs is that HCWs may transmit certain bloodborne viruses to their patients (or vice versa) if their blood comes into contact with the patient’s open tissues (CDNA 2019).
These viruses include:
(CDNA 2019)
Likelihood of Bloodborne Disease Transmission During an Exposure Prone Procedure
| Mode of transmission | Risk of infected HCW to patient transmission | Risk of infected patient to HCW transmission | |
|---|---|---|---|
| Hepatitis B virus |
|
0.2% to 13.19% | 1% to 62% (depending on the patient’s hepatitis B e-antigen status) |
| Hepatitis C virus |
|
0.04% to 4.35% | 0% to 7% |
| Human immunodeficiency virus (HIV) | 0.0000024% to 0.000024% | 0.3% |
(Adapted from CDNA 2019)
There have only been four cases worldwide of HIV transmission to patients during EPPs. In all of these cases, the HCW was not taking antiretroviral therapy (CDNA 2019).
Recommendations for Healthcare Workers
In general, all HCWs should be aware of their BBV status and take reasonable precautions to avoid transmission. Those who are at risk of contracting a BBV outside of work should seek regular testing (CDNA 2017).
Furthermore, all HCWs (including students) are expected to be vaccinated against hepatitis B before commencing their employment (CDNA 2017).
Read: Workforce Immunisation for Healthcare Staff
Those who perform EPPs should be tested for bloodborne viruses at least once every three years and should seek follow-up care and testing in a timely manner if they have potentially been exposed to a BBV occupationally or outside of work (CDNA 2018).
BBVs may be asymptomatic or mild, meaning that a HCW who has not been tested may not be aware that they have contracted a BBV (CDNA 2018).
Risk Factors for Blood or Body Fluid Exposure
- Being injected with over 1 mL of blood or body fluid
- Parenteral exposure to laboratory specimens containing a high concentration of a BBV
- Suffering a skin-penetrating injury, including:
- Injury from a needle that is contaminated with blood or body fluid
- Injury that results in bleeding and is caused by an instrument that is visibly contaminated with blood or body fluid
- Injury that causes the mucous membrane or conjunctival contact to come into contact with blood
- Injury from a human bite or scratch where there is exposure to blood or body fluid infectious for a BBV
- Direct contact between non-intact skin and blood or body fluid
- Direct vaccination with HIV tissue or material, or material likely to contain HIV, HBV or HCV (in laboratory settings).
(Queensland Health 2024)
Management of Exposures to Blood and Body Fluid

If you are exposed to blood or body fluid, immediate steps should be taken:
Note: Always adhere to your organisation’s policies and procedures.
- Wash any skin areas (including wounds and non-intact skin) that have come into contact with blood or body fluid using soap and water.
- Avoid squeezing or rubbing the affected area.
- If the eyes or mucous membranes have been exposed:
- Irrigate using water or normal saline
- If the eyes are contaminated, rinse them while open for at least 30 seconds (remove any contact lenses first).
- If blood or bodily fluids have entered the mouth, spit them out and rinse the mouth out with water multiple times, spitting the water out each time.
- Remove any contaminated clothing and shower if required.
(Queensland Health 2024; SA Health 2023)
Documentation is crucial after an incident of exposure has occurred. It should include:
- Information about the exposure:
- Date and time of the exposure
- Type of exposure, including site, blood or body fluid involved, and first aid performed
- Type of injury sustained from the incident
- Information about the object that caused the injury (e.g. the gauge of the needle)
- Type of body fluids involved
- The volume of blood or body fluid the person was exposed to
- Information about the source person:
- BBV status
- Demographic factors that may increase the risk of BBV infection
- Information about the exposed person:
- Status of the exposed person with respect to BBVs, including vaccination status
- Pregnancy risk and lactation
- Medical history.
(Queensland Health 2024)
What Happens if a Healthcare Worker Tests Positive for a Bloodborne Virus?
A HCW who tests positive for a BBV must stop performing EPPs immediately (CDNA 2017).
They will be allowed to resume performing EPPs if they:
- Seek ongoing and appropriate medical care for the BBV
- Undergo testing for viral load levels
- Maintain viral load levels that comply with the criteria stated in CDNA Guidelines
- Undergo any required treatment as stated in the CDNA Guidelines, and
- Comply with other relevant criteria as stated in the CDNA Guidelines.
(CDNA 2017)
The pathway for resuming EPPs after a BBV diagnosis is as follows:
Note: Always adhere to your organisation’s policies and procedures.
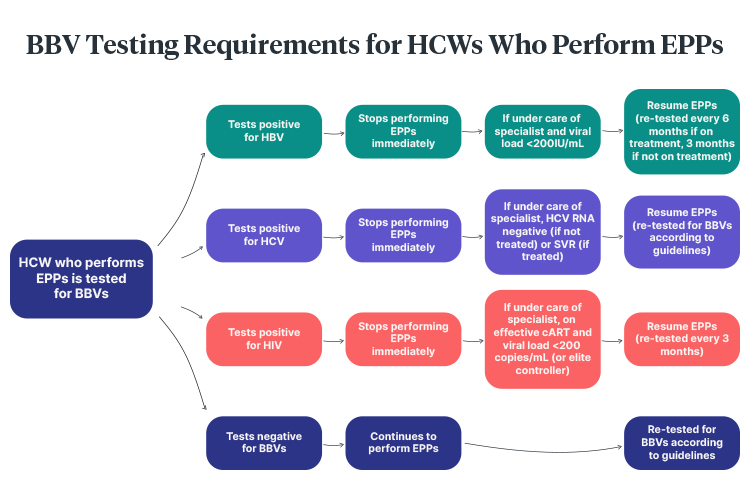
Note: False positives for BBV are possible but very rare, as screening involves a two-step testing process (CDNA 2017).
Patient Exposure to Blood or Body Fluid From a Healthcare Worker With a BBV
Note: Always adhere to your organisation’s policies and procedures.
If this occurs, a comprehensive risk assessment should be performed in consultation with the HCW’s treating practitioner. This risk assessment should comprise:
- The significance of the exposure
- The exposed patient’s status
- The HCW’s BBV status, including:
- Current viral load
- BBV history
- Adherence to treatment
- Frequency and severity of fluctuations in viral load
- Any factors that might increase viral load.
(CDNA 2019)
If there is any concern that the HCW’s viral load is above the allowed level, the HCW should be tested immediately. Post-exposure prophylaxis and any other follow-up should be offered to the patient based on local policies (CDNA 2019).
Test Your Knowledge
Question 1 of 3
True or false: All healthcare workers living with a bloodborne virus are permanently prevented from performing exposure prone procedures.
Topics
Further your knowledge
 Free
Free Free
Free Free
Free Free
Free Free
FreeReferences
- Communicable Diseases Network Australia 2017, CDNA Guidance on Classification of Exposure Prone and Non-exposure Prone Procedures in Australia 2017, Australian Government, viewed 10 February 2025, https://www.health.gov.au/resources/publications/cdna-guidance-on-classification-of-exposure-prone-and-non-exposure-prone-procedures-in-australia-2017?language=en
- Communicable Diseases Network Australia 2018, Information for Healthcare Workers Who Perform Exposure Prone Procedures Who are NOT Living With a Blood Borne Virus, Australian Government, viewed 10 February 2025, https://www.health.gov.au/resources/publications/cdna-national-guidelines-information-for-healthcare-workers-who-perform-exposure-prone-procedures-who-are-not-living-with-a-blood-borne-virus?language=en
- Communicable Diseases Network Australia 2019, Australian National Guidelines for the Management of Healthcare Workers Living with Blood Borne Viruses and Healthcare Workers Who Perform Exposure Prone Procedures at Risk of Exposure to Blood Borne Viruses, Australian Government, viewed 10 February 2025, https://www.health.gov.au/resources/publications/cdna-national-guidelines-healthcare-workers-living-with-blood-borne-viruses-perform-exposure-prone-procedures-at-risk-of-exposure-to-blood-borne-viruses?language=en
- Nursing and Midwifery Board of Australia 2021, Fact Sheet: Exposure-prone Procedures - Registration and Renewal Declaration, Ahpra, viewed 10 February 2025, https://www.nursingmidwiferyboard.gov.au/Registration-and-Endorsement/Registration-Renewal/fact-sheet-exposure-prone-procedures.aspx
- Queensland Health 2024, Management of Occupational Exposure to Blood and Body Fluids – Infection Prevention and Control, Queensland Government, viewed 10 February 2025, https://www.health.qld.gov.au/__data/assets/pdf_file/0032/1398191/qh-gdl-321-8.pdf
- SA Health 2023, Handling Blood and Other Body Substances, Government of South Australia, viewed 10 February 2025, https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/conditions/infectious+diseases/handling+blood+and+other+body+substances
Additional Resources
- ASHM Testing Portal | ASHM
- Australian National Guidelines for the Management of Healthcare Workers Living with Blood Borne Viruses and Healthcare Workers Who Perform Exposure Prone Procedures at Risk of Exposure to Blood Borne Viruses | CDNA
- Guidance on Classification of Exposure Prone and Non-exposure Prone Procedures in Australia 2017 | CDNA
- Management of Occupational Exposure to Blood and Body Fluids – Infection Prevention and Control | Queensland Health