How does a patient die from sepsis? What happens to their body, vessels and organs?
When someone experiences an infection, every cell of their body is compromised. With the right clinical assessment skills and knowledge, it’s possible to identify sepsis early and save lives.
This article has been updated to reflect the Surviving Sepsis Campaign Guidelines 2021 and Sepsis Clinical Care Standard.
Note: This article is intended as a refresher and should not replace best-practice care. Always refer to your local policy on recognising and responding to sepsis.
What is Sepsis?
Sepsis is an overactive response to an infection that causes the body to damage its own organs and tissue (Sepsis Alliance 2022).
Sepsis can be caused by any infectious pathogen (Mayo Clinic 2023).
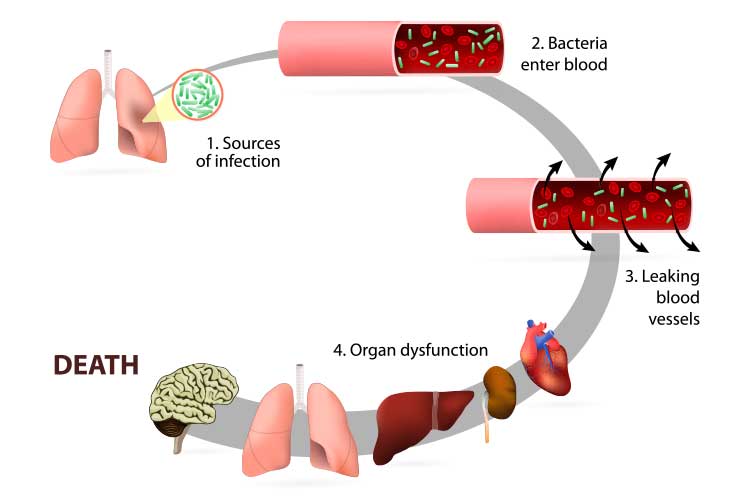
In sepsis, an infection causes the body to release immune chemicals into the systemic circulation, triggering a widespread inflammatory process that causes coagulation (blood clotting) and hypoperfusion (decreased blood supply to the organs). This impaired blood supply starves the organs of oxygen, causing significant damage (NIGMS 2024).
Sepsis is a life-threatening medical emergency that can lead to septic shock, multiple organ failure and potentially death.
Every year, sepsis is estimated to affect 55,000 Australians, resulting in at least 8,700 deaths (ACSQHC 2022a).
Who is at Risk of Sepsis?
Sepsis can affect anyone. However, those at increased risk include:
- Older people
- Neonates and young children
- Aboriginal and Torres Strait Islander people
- People living with complex health issues
- People who have COVID-19
- People who are immunocompromised
- Pregnant people
- People who have just given birth
- People receiving chemotherapy for cancer treatment
- People who have burns, wounds or injuries
- People who have previously experienced sepsis.
(ACSQHC 2022b)
Signs of Sepsis
The many possible signs and symptoms of sepsis include:
- Increased respiratory rate or breathlessness
- Fever and chills
- Low body temperature
- Decreased urine output
- Increased heart rate
- Nausea and vomiting
- Diarrhoea
- Fatigue, sleepiness or confusion
- Severe pain
- Feeling ‘worse than ever’.
(ACSQHC 2022b)
Children may present with:
- Increased respiratory rate or long lapses in breathing
- Discoloured or blotchy skin
- Abnormally cold skin
- Non-blanching rash
- Decreased urine output (e.g. less frequent wet nappies)
- Drowsiness, confusion or difficulty waking up
- Restlessness
- Floppiness
- Vomiting
- Convulsions
- Severe, unexplained pain.
(ACSQHC 2022b)
Recognising Sepsis
There are a variety of tools available to support the early recognition of sepsis. The Sepsis Clinical Care Standard states that no single tool is applicable to all population groups and clinical settings. Therefore, screening methods should be chosen based on factors such as the patient’s age and the care setting. Suitable tools for adults include:
- Lactate-enhanced qSOFA (LqSOFA)
- National Early Warning Score (NEWS)
- Modified Early Warning Score (MEWS).
(ACSQHC 2022b)
For paediatric patients, standardised graphic observation charts such as the Children’s Early Warning Tool (CEWT) may be used to aid in the recognition of sepsis (ACSQHC 2022b).
Note: Use of the Quick Sequential Organ Failure Assessment (qSOFA) and Systemic Inflammatory Response Syndrome (SIRS) tools is not recommended (ACSQHC 2022b).
Responding to Suspected Sepsis
Sepsis is an emergency that requires timely intervention. If sepsis is suspected, a locally approved clinical pathway should be activated immediately (ACSQHC 2022b).
The Surviving Sepsis Campaign is an international initiative aimed at reducing the global mortality of sepsis. Their Hour-1 Bundle guideline sets out five tasks that should be commenced (though may not necessarily be finished) within the first hour of sepsis recognition as part of initial resuscitation. They are:
- Measure the patient’s lactate level. Elevated lactate levels can signal either a protective or harmful response to shock and are useful in screening for conditions like sepsis. While not diagnostic on their own, lactate tests are simple, aid in early recognition of sepsis in deteriorating patients, and should be routinely considered to help prevent serious harm or death.
- Remeasure lactate if the initial level is elevated (> 2 mmol/L).
- Obtain blood cultures.
- Administer broad-spectrum antibiotics within the first hour if infection is suspected. Antimicrobial therapy should be given as early as possible to patients with sepsis, as delays in the first dose are linked to higher mortality.
- Begin rapidly administering crystalloid as per your organisation's policy.
- Consider administering vasopressors if hypotensive during or after fluid resuscitation to maintain a mean arterial pressure ≥ 65 mm Hg.
- Vasopressors must be administered by a medical practitioner. The administration of this medicine should be considered in a critical care environment, however, if the patient is hypotensive, the objective is to maintain perfusion to all vital organs. Therefore, continuous blood pressure monitoring is imperative. The frequency of observation should be increased.
(SCCM 2019; ACSQHC 2022b)
Sepsis and septic shock are medical emergencies. It is imperative that you act quickly and minimise the amount of time spent before commencing treatment. You must perform a thorough head-to-toe assessment and investigate any obvious signs of infection, increasing the frequency of observations and assessing whether the patient is responding to treatment (e.g. fluid resuscitation). You must inform colleagues about the patient’s status during handovers (SCCM 2019).
You should be able to locate the Surviving Sepsis Campaign’s guidelines at any time, along with your organisation’s own policies and protocols.

Complications of Sepsis
Untreated sepsis can cause the patient’s blood pressure to drop dramatically, causing it to progress into septic shock. The organs are starved of an adequate blood supply, resulting in hypoperfusion and leading to multiple organ dysfunction syndrome. This is an extremely severe condition that can lead to fatality (Healthdirect 2024).
If the early signs of sepsis have not been identified, the patient can deteriorate rapidly, requiring basic life support. Call for assistance as per hospital protocol. Remember to act quickly to save lives.
Post-Sepsis Outcomes
Only about 70% of people diagnosed with sepsis will survive, and of those survivors, 50% will develop post-sepsis syndrome (Sepsis Alliance 2022). This can be caused by a variety of factors, including any resulting permanent disability from the sepsis and also the psychological effects of both the illness and their prolonged hospitalisation.
Symptoms of Post-Sepsis Syndrome
Post-sepsis syndrome may involve a range of physical and/or psychological symptoms, including:
- Insomnia
- Nightmares, vivid hallucinations and panic attacks
- Shortness of breath
- Disabling muscle and joint pains
- Oedema in the limbs
- Subsequent infections
- Extreme fatigue
- Reduced appetite
- Decreased organ function
- Hair loss
- Rash
- Poor concentration
- Decreased cognitive functioning
- Loss of self-esteem and self-belief
- Hallucinations
- Panic attacks
- Flashbacks
- Depression
- Mood changes
- Impaired memory
- Post-traumatic stress disorder (PTSD).
(Sepsis Alliance 2024)
Following recovery from sepsis, healthcare professionals must ensure that the patient’s treatment takes a holistic approach. This is essential as the individual may be feeling not only the physical effects of being ill, but also the psychological and cognitive effects of experiencing sepsis and social isolation following a prolonged hospital stay.
Test Your Knowledge
Question 1 of 3
Why is early administration of broad-spectrum antibiotics critical in suspected sepsis cases?
Topics
Further your knowledge
References
- Australian Commission on Safety and Quality in Health Care 2022a, Media Backgrounder – What is Sepsis and How Can We Avoid This Silent Killer?, Australian Government, viewed 8 May 2025, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/media-backgrounder-what-sepsis-and-how-can-we-avoid-silent-killer
- Australian Commission on Safety and Quality in Health Care 2022b, Sepsis Clinical Care Standard, Australian Government, viewed 8 May 2025, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/sepsis-clinical-care-standard-2022
- Healthdirect 2024, Sepsis, Australian Government, viewed 8 May 2025, https://www.healthdirect.gov.au/sepsis-septicaemia
- Mayo Clinic 2023, Sepsis, Mayo Clinic, viewed 8 May 2025, https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214
- National Institute of General Medical Sciences 2024, Sepsis, U.S. Department of Health & Human Services, viewed 8 May 2025, https://www.nigms.nih.gov/education/fact-sheets/Pages/sepsis
- Sepsis Alliance 2022, What is Sepsis, Sepsis Alliance, viewed 8 May 2025, https://www.sepsis.org/sepsis-basics/what-is-sepsis/
- Sepsis Alliance 2024, Post-Sepsis Syndrome, Sepsis Alliance, viewed 8 May 2025, https://www.sepsis.org/sepsis-basics/post-sepsis-syndrome/
- Society of Critical Care Medicine 2019, Hour-1 Bundle: Initial Resuscitation for Sepsis and Septic Shock, SCCM, viewed 8 May 2025, https://sccm.org/SCCM/media/SCCM/PDFs/Surviving-Sepsis-Campaign-Hour-1-Bundle.pdf?_gl=1*16byuw7*_gcl_au*NDk0MTgyMTczLjE3NDY2NjQyNTI.


