It starts off as something simple. Your patient is complaining of leg pain. One leg is swollen to twice the size of the other and is bright red. Whether your patient has had surgery, suffered trauma, or has even just come off of a long trip in the car, they may be at risk of venous thromboembolism (VTE), also known as deep vein thrombosis (DVT).
It’s important to constantly monitor patients for signs and symptoms of VTE and be adequately informed about prevention measures. The prophylaxis for VTE has come a long way in recent years. Hospitals now have dedicated assessments in place to help prevent this sometimes silent condition from taking lives.
Symptoms of Venous Thromboembolism
Although most nurses are trained to look for swelling in one arm or leg compared to the other, as many as 30% of VTE cases do not present this way (Waheed et al. 2023).
Another sign of VTE is pain upon quick dorsiflexion of the foot. This is known as Homan's sign, and can sometimes tip off a nurse to possible VTE. However, note that Homan's sign is absent in half of all VTE cases and may sometimes indicate other conditions (Patel 2019).
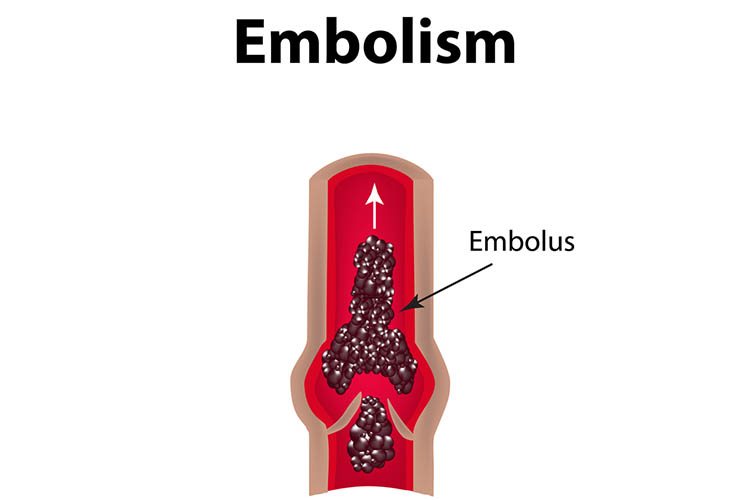
Sometimes, the only way to know the patient has had a deep vein thrombosis is if they start showing signs of a pulmonary embolism (PE). A PE is a clot that travels from another part of the body to the lungs. Some signs of PE include shortness of breath, pleuritic chest pain, an increased breathing rate and coughing up blood. However, a PE may have no signs or symptoms either, and the patient may suddenly go into cardiac arrest. This is why prevention is the most important step in treating VTE.
Risk Factors for Venous Thromboembolism
It's important to recognise the patients who are at higher risk of VTE. These patients include:
- Surgical patients
- Trauma patients
- Patients with IVs in situ
- Patients who require injections of irritating substances
- Patients with a history of IV drug abuse
- Patients with history of prior VTE
- Patients who are immobilised for more than three days
- Patients who have compression of the iliac or femoral veins
- Patients with a history of congestive heart failure
- Pregnant patients
- Patients undergoing hormone therapy
- Patients who are malignant
- Patients who have coagulation issues
- Patients who are dehydrated.
Prevention of Venous Thromboembolism
There are many nursing interventions that can be performed to prevent VTE.
Early ambulation following surgery is absolutely vital to assist in the mobilisation of blood in the legs to prevent clots. Turning and positioning immobilised patients every two hours can also help prevent clots. Compression stockings are important for those who are bed-bound, as they help massage the legs and keep blood flowing to prevent VTEs from forming. The important point to remember with these interventions is that all staff must be trained in how to use them, and should be instructed to put them on the patient when they are lying in bed. Using a combination of nursing interventions and pharmacological aids is your best chance of stopping VTEs before they harm your patient.
Topics
References
- Patel, K 2019, Deep Venous Thrombosis (DVT) Clinical Presentation, Medscape, viewed 23 November 2023, https://emedicine.medscape.com/article/1911303-clinical#b3
- Waheed, SM, Kudaravalli, P & Hotwagner, DT 2023, ‘Deep Vein Thrombosis’, StatPearls, viewed 23 November 2023, https://www.ncbi.nlm.nih.gov/books/NBK507708/
 New
New 