What is Credentialing?
Credentialing is the process of systematically verifying the qualifications, experience, professionalism, and competence of healthcare practitioners. It is essential for ensuring that healthcare providers are adequately qualified to perform their roles within a healthcare setting.
What is Scope of Clinical Practice?
The scope of clinical practice defines the specific services and activities that a healthcare practitioner is authorised to perform, based on their credentials, training, and competence. It ensures that patients receive care from practitioners who are equipped with the necessary skills and knowledge.
Importance of Credentialing and Scope of Clinical Practice
Credentialing and clearly defining the scope of clinical practice are crucial for maintaining high standards of patient care. They help to minimise clinical risks and ensure that healthcare services are provided safely and effectively by qualified professionals.
Examples of Credentialing and Scope of Clinical Practice
Examples include verifying a surgeon's qualifications and experience before granting privileges to perform specific surgical procedures, or accrediting a nurse to administer certain types of medication based on their training and competence.
What is the "Credentialing and Scope of Clinical Practice" Training Requirement?
Training for credentialing and scope of clinical practice involves understanding regulatory requirements, the process of verifying qualifications, and the mechanisms for defining and reviewing a practitioner's scope of practice.
Relevant Standards
The organisation has processes in place to:
- Defines clinician's scope of clinical practices, considers the clinical service capactiy of the organisation and the services plan
- Monitor the practice of clinicians ensuring they're operating within the defined scope of clinical practice
- Regularly review the clinician's scope of clinical practice, and wheneber a new clinical service, procedure or technology is. introduced or altered substantially
The organisation:
- Has processes to ensure clinicians are credentialed (where relevant)
- Monitors the effectriveness of the credentialing process, and improves it where necessary
National Safety and Quality Health Service (NSQHS) Standards
Failure to comply with the requirements could lead to an organisation being penalised or reprimanded.
What Skills Do Staff Need for Credentialing and Scope of Clinical Practice?
The effectiveness of credentialing and managing the scope of clinical practice hinges on a robust skill set that encompasses a wide range of competencies from regulatory knowledge to interpersonal communication:
| Skill | Description |
|---|---|
| Understanding of Healthcare Regulations | Proficiency in national, state, and local healthcare regulations, including specific knowledge of NSQHS Standards, is essential for ensuring compliance and safeguarding patient safety. |
| Critical Evaluation and Verification | The ability to critically assess, verify, and evaluate the credentials, training, and professional history of healthcare practitioners to uphold high standards of care |
| Risk Management | Skills in identifying, assessing, and managing potential risks associated with the scope of clinical practice to minimise patient safety hazards. |
| Effective Communication | The capability to communicate clearly and effectively with a diverse range of stakeholders, including healthcare professionals, regulatory bodies, and patients, to facilitate understanding and compliance with scope of practice parameters. |
| Negotiation and Conflict Resolution | Proficiency in negotiating scope of practice boundaries and resolving any conflicts that arise during credentialing processes. |
| Decision Making | The ability to make informed decisions based on a comprehensive evaluation of available information and potential outcomes. |
| Empathy | Helps in understanding patient concerns and fears, especially in stressful situations where identification errors can escalate anxiety. |
How to Assess Staff in Credentialing and Scope of Clinical Practice
Effectively assessing staff competency in credentialing and scope of clinical practice is a multi-faceted process that requires a strategic approach:
- Self-Assessments: Encourage healthcare professionals to conduct self-assessments to reflect on their understanding and application of credentialing and scope of practice guidelines.
- Peer Reviews: Utilise peer review mechanisms where colleagues assess each other’s competency, providing a platform for feedback and continuous improvement.
- Performance Evaluations: Regularly scheduled performance evaluations by supervisors or credentialing committees to assess practical application of skills and knowledge.
- Case Studies and Simulation: Engagement with real-life case studies and simulation exercises to test the ability to apply knowledge in practical scenarios and make informed decisions.
- Continuous Professional Development Tracking: Implementing systems to track continuous professional development activities and their impact on practice.
Strategies to Support Healthcare Staff Develop Skills in Credentialing and Scope of Clinical Practice
Supporting employees in enhancing their skills requires a proactive and comprehensive strategy that includes:
- Structured Training Programs: Offering structured training programs that cover the foundational aspects, as well as the latest developments in credentialing and scope of clinical practice.
- Mentorship and Coaching: Establishing mentorship and coaching programs where less experienced staff can learn from seasoned professionals through one-on-one sessions or group discussions.
- Access to Resources: Providing easy access to a variety of resources, including online courses, webinars, professional literature, and guidelines on best practices in credentialing and scope management.
- Feedback and Performance Improvement Plans: Implementing a robust feedback system that not only identifies areas for improvement but also offers personalised performance improvement plans.
- Encouraging Professional Development: Encouraging and facilitating participation in external conferences, workshops, and seminars that focus on credentialing and scope of clinical practice.
- Creating Learning Communities: Promoting the formation of learning communities within the organisation to foster a culture of continuous learning and knowledge sharing.
Sample Training Plan for the "Credentialing and Scope of Clinical Practice" Requirement
Below is a skills assessment that to identify gaps in staff knowledge that a training plan can be created for:
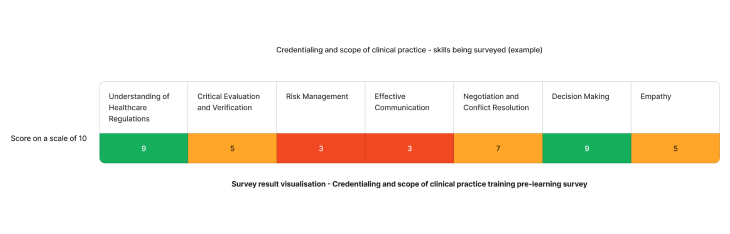
Using the above needs assessment survey as an example - The skill requiring the most attention for credentialing and scope of clinical practice in healthcare are risk management and communicationskills. We can target learning initiatives to fill these gaps to enhance staff competency.
Need an LMS that can support credentialing and scope of clinical practice skills?
Contact Ausmed today and see how we can support with your training requirement needs!
Staff Competency Assessment for Credentialing and Scope of Clinical Practice - Example
Consider the following survey questions to evaluate staff's knowledge in credentialing and scope of clinical practice.
Staff Survey - Credentialing and Scope of Clinical Practice Competency
-
How would you verify the credentials of a healthcare practitioner applying for accreditation in a new area of practice?
- [Answer here]
-
Describe a situation where you had to define or revise the scope of clinical practice for a healthcare professional. How did you approach it?
- [Answer here]
-
What strategies would you employ to ensure compliance with NSQHS Standards related to credentialing and scope of practice?
- [Answer here]
-
Can you provide an example of how you have dealt with a discrepancy in a practitioner's claimed qualifications or experience?
- [Answer here]
Conclusion
Developing a comprehensive training program for credentialing and scope of clinical practice is essential for maintaining the integrity and quality of healthcare services. By focusing on the necessary skills, providing adequate training, and continuously assessing competency, healthcare organisations can ensure that their staff are well-equipped to manage these critical aspects of healthcare delivery.
References
- Australian Commission on Safety and Quality in Health Care, 2023. 'Clinical Governance Standard'
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS Action 1.23'
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS Action 1.24'