What is Documentation?
Documentation refers to the systematic record-keeping of individual cases to facilitate better decision-making, care planning, and legal compliance (Australian Commission on Safety and Quality in Health Care, 2023). It serves as written evidence of all interactions and interventions between healthcare providers and clients.
Why is Documentation Important in Healthcare?
Documentation in healthcare serves a multitude of purposes that contribute to the overall quality and safety of patient care.
- Communication: Comprehensive and accurate records serve as a communication bridge among healthcare providers, ensuring that everyone involved in a patient’s care has access to the same information.
- Legal Compliance: Documentation serves as a legal record of all clinical actions taken, protecting healthcare providers in the case of legal scrutiny.
- Quality Assurance: Consistent and accurate documentation is key to quality audits, performance assessments, and clinical governance activities. It enables healthcare organisations to assess and improve their service quality.
- Decision-Making: Well-maintained records assist in clinical decision-making by providing a comprehensive view of the patient’s history, current condition, and past treatments.
What is the Documentation Training Requirement?
Documentation training in Australian healthcare organisations should be meticulously aligned with the National Safety and Quality Health Service (NSQHS) standards, specifically Action 6.11, Aged Care Quality Standards 2.3(d) and 3.3(e), and the Strengthened Aged Care Quality Standards, particularly Standard 1.3.1 (Aged Care Quality and Safety Commission, 2023). These standards mandate stringent guidelines for effective client documentation to ensure safe and quality healthcare services.
Relevant Standard
Action 6.11: Documentation of information.
- Record-Keeping Protocols: The training should focus on making sure that all healthcare professionals correctly document clinical information, including Critical information, alerts and risks, reassessment processes and outcomes, changes to the client care plan.
- Policy availability: Any documentation policies recorded and created by the organisations must be made readily available for the workforce to understand.
- Communication: Roles and responsibilities expected of the workforce must be communicated and understood to ensure adherence.
National Safety and Quality Health Service (NSQHS) Standards
- Assessment and planning are communicated to the client and documented effectively
- Services plans are readily available for the consumer
- Client conditions, preferences and needs are communicated and documented within the organisation
- Client condition, preferences and needs are communicated and documented for others that share responsibility of care
Action 1.3.1: Effective client (older person) documentation
- Information provided to clients and residents must be up-to-date, accurate and presented in a timely manner
- Communicated in a manner that the client can understand
- Reinforces the ability for the client to make informed decisions about their care.
Strengthened Quality Standards framework analysis - Aged Care Quality Standards
Failure to comply with the requirements could lead to an organisation being penalised or reprimanded.
What Skills Do Staff Need for Effective Documentation in Healthcare?
| Skill | Key Elements |
|---|---|
| Attention to Detail |
Staff must ensure the accurate recording of clinical information. Factual errors can lead to ineffective treatment plans and potentially harm patients. |
| Digital Proficiency |
With the increasing adoption of Electronic Health Records (EHR), digital literacy is essential. Staff must be able to navigate EHR systems effectively to update and retrieve patient information. |
| Communication Skills |
Documentation is not merely an administrative task; it is a form of clinical communication. Staff need to be skilled in conveying information clearly and concisely to ensure effective team collaboration. |
| Ethical Awareness |
A good understanding of the ethical principles, especially around patient confidentiality and data security, is essential. |
| Time Management |
The healthcare setting is often fast-paced, and professionals must balance the urgency of patient care with the necessity of thorough documentation. |
By supporting staff in developing these skills, they will be better equipped to engage and learn and apply documentation best-practice within your organisation, and supporting improved patient outcomes.
How to Assess Staff Competency in Documentation
Ensuring that healthcare staff are competent in documentation is crucial for maintaining high standards of care and legal compliance.
Methods of Assessing Staff Competency in Documentation
Staff competency can be assessed in the following methods:
- Observational Audits:
Supervisors or peer reviewers may observe staff during their documentation process to evaluate compliance with established protocols and guidelines. - Peer Reviews:
Colleagues review each other’s documentation for accuracy, comprehensiveness, and adherence to legal and ethical standards. - Written Tests:
Staff may be asked to complete written assessments that evaluate their understanding of documentation protocols, including scenarios that test their application of NSQHS and Aged Care Quality Standards. - Quality Audits:
Periodic internal audits can help identify areas for improvement and ensure continuous adherence to Australian healthcare standards. - Surveys:
Internal surveys to staff assessing their competency on key elements of documentation in relation to the NSQHS and Aged Care Quality Standards.
Strategies to Support Healthcare Staff Improve Documentation Skills
Improving documentation is an ongoing endeavour that should align with the relevant standards and aim to improve staff competency. The following are strategies to improve documentation within healthcare settings:
- Regular Training: Frequent workshops, webinars, or online courses can help keep the staff updated with the latest best practices and regulations regarding documentation.
- Use of Standardised Templates: Standardised templates can make the documentation process more uniform and easier to follow, ensuring that essential elements are not overlooked.
- Implement Checklists: Checklists serve as quick reminders and can be particularly useful in ensuring that all essential details have been documented. This can be especially beneficial during busy shifts or emergencies.
- Peer Review Mechanisms: Encourage peer reviews of documentation as an additional layer of oversight, promoting adherence to Australian healthcare standards.
- Technology Integration: Utilising software that can cross-verify information can help reduce errors and enhance the quality of documentation. However, staff should be well-trained to use such technology effectively.
- Regular Audits: Periodic internal and external audits can provide valuable insights into the areas that need improvement and also ensure ongoing compliance with national standards.
Sample Training Plan for the Documentation Training Requirement
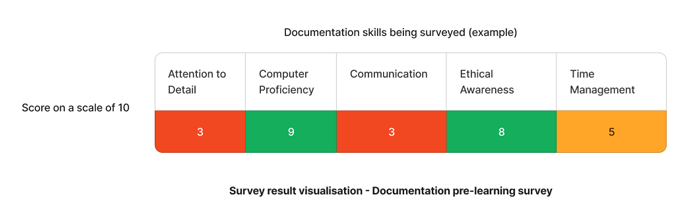
Using the above image as an example - The results that require immediate attention are "attention to detail" and "communication" skills.
Based on this, we can support these workers to better develop their documentation skills. Below is a sample training plan that can be adapted to your organisation's specific needs.
| Quarter | Topics | Resources |
|---|---|---|
| Q1 | Attention to detail |
|
| Q2 | Communication |
Need documentation training for your staff?
Contact Ausmed today and see how you can enhance your staff's provision of care!
Staff Competency Assessment for Documentation - Example
Staff assessments are essential for organisations and learning managers to perform in order to determine the skills gaps staff may have to develop a comprehensive training plan relating to documentation.
Staff Survey - Documentation Competency
-
What are the key components of effective documentation?
[Write your response here]
-
How do you ensure confidentiality in client documentation?
[Write your response here]
-
How proficient are you in using electronic health record systems?
[Write your response here]
-
What strategies do you use to maintain accuracy in documentation?
[Write your response here]
-
How do you handle corrections or amendments in client documentation?
[Write your response here]
Conclusion
Effective documentation is the cornerstone of quality healthcare, fulfilling both legal and clinical imperatives. Ensuring that staff are well-trained and competent in documentation is essential for maintaining high standards of patient care. Adherence to NSQHS Action 6.11, Aged Care Quality Standards 2.3(d) and 3.3(e), and the Strengthened Aged Care Quality Standards 1.3.1 ensures compliance and the continuous improvement of healthcare services in Australia.
References
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Communicating for Safety Standard'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 6.11 - Documentation of information.'
- Aged Care Quality and Safety Commission, 2023. 'Stronger Standards, Better Aged Care Program - Action 1.3.1'



