This article is part of our Training Requirement Series where we provide comprehensive guides to meet the actual training requirements that are often needed/requested of learning and development departments within Australia's healthcare organisations. This series includes both general requirements, such as infection prevention and control, but also focuses on the specific requirements stemming from the NDIS, Aged Care and NSQHS Quality Standards.
What is Infection Prevention?
Infection prevention refers to the policies, procedures, and practices put in place to minimise the risk of transmitting infections within healthcare settings. It is integral to patient safety and is an essential consideration for healthcare staff.
What is the NSQHS Infection Prevention Training Requirement?
According to NSQHS, infection prevention training is necessary to meet a range of actions including Actions 3.05-3.09, Actions 3.13-3.16, and Actions 3.18-3.19 . This training encompasses topics such as the appropriate use of personal protective equipment (PPE), environmental cleaning, infection prevention systems, and more.
Relevant Standards
Action 3.05: Infection Surveillance Strategies
Organisations providing services should use strategies for infections, risk of infection, and antimicorbial use that:
- Is implemented in a timely manner incorporating national and jurisdictional information
- Collects healthcare-associated and other infections data relevant to the size and scope of the organisation
- Reduces infections associated risks by reporting on surveillance data on infection to the workforce
- Supports antimicrobial prescribing via monitoring, assessing and using surveillance data
- Monitors risk responsiveness identified by surveillance
- Reports surveillance data on antimicrobial use to the workforce, governing body, consumers and other relevant groups
- Organisations have process to apply stansmission-based and standard precautions consistent with the current addition of the Australian Guidelines for the Prevention and Control of Infection in Healthcare, as well as jurisdictional requirements, laws and policies (including work health and safety laws)
Action 3.07: Healthcare organisation standard and transmission-based precautions
Healthcare organisations must have:
- Employ cooperative methods to evaluate and communicate potential infection hazards to both patients and healthcare staff.
- Implement a multifaceted approach to minimize infection spread, utilising the hierarchy of controls to make it as effective as feasibly possible.
- Establish clear guidelines for the proper selection, usage, testing, and fitting of Personal Protective Equipment (PPE) among the workforce.
- Implement systems to stay on top of and adapt to emerging scientific insights, as well as national or jurisdictional regulations, policies, and guidelines related to infection control.
- Outline methods to audit adherence to both standard and transmission-based precautions for infection prevention.
- Develop mechanisms to evaluate the proficiency of healthcare staff in the application of standard and transmission-based precautions.
- Introduce systems and training to boost compliance levels with standard and transmission-based precautionary measures.
Action 3.08: Workforce Applying standard and transmission-based precautions
Healthcare workforce staff should:
- Evaluate patients' infection risks at the point of referral, upon admission, and at different stages during their healthcare journey.
- Determine if a patient is carrying a contagious illness, or has existing or prior colonisation with significant organisms, either locally or nationally.
- Assess the specific needs for patient accommodation to effectively manage and mitigate infection risks.
- Evaluate the potential impacts on a patient’s wellbeing when isolated for infection control.
- Implement controls related to heating, ventilation, water systems, facility design, and workflow to minimise infection risks.
- Outline the necessary precautions when moving a patient either within the healthcare facility or to external services.
- Identify when extra environmental cleaning or disinfection procedures and resources are needed.
- Assess the specific infection risks associated with the medical procedure being carried out.
- Determine the types of equipment needed for everyday care while adhering to infection control guidelines.
Action 3.09: Standard and transmission-based precaution processes
Helathcare organisations have processes to
- Assess and act upon data concerning infections within the community that could affect both patients and healthcare staff.
- Share pertinent information about a patient's infectious condition during their care and at transitions between different levels or settings of care.
- Supply the patient, their family, and carers with essential details about their infectious status, the risks involved, and the precautions needed to limit infection spread.
Action 3.13: Maintaining a clearn and safe environment
Processess in place in line with the Australian Guidelines for the Prevention and Control of Infection in Healthcare and jurisdictional to:
- Take action to mitigate risks posed by environmental factors and newly identified infections.
- Utilise cleaning and disinfection products that are listed on the Australian Register of Therapeutic Goods, and adhere to the manufacturers' usage guidelines and recommended schedules.
- Ensure that staff have access to training modules that cover standard cleaning processes, outbreak-related cleaning, and procedures for dealing with new types of infections.
- Regularly assess the efficacy of cleaning practices and adherence to the organisation's environmental cleaning policies.
- Use audit outcomes to enhance environmental cleaning protocols and compliance with organisational policy.
Action 3.14: Clean and safe environment evaluation and response
Processes to:
- Evaluate both new and existing equipment, devices, and products utilised within the healthcare organisation for infection risk.
- Extend infection prevention measures to cover both clinical and non-clinical zones, as well as employee amenity spaces.
- Include procedures for the upkeep, repair, and enhancement of buildings, equipment, furnishings, and fittings, with infection control in mind.
- Implement guidelines for the safe handling, transportation, and storage of linen to minimise infection risks.
- Plan for novel infections and risks that emerge as part of coordinated public health responses or pandemic preparedness.
Action 3.15: Workforce screening and immunisation
Organisations have risk-based workforce vaccine-preventable diseases immunisation and screening policies that:
- Ensure that protocols are in line with the latest edition of the Australian Immunisation Handbook.
- Adapt measures to be consistent with jurisdiction-specific guidelines concerning vaccine-preventable diseases.
- Address particular infection risks that could impact the healthcare workforce, consumers, and patients.
Action 3.16: Workplace infections proceses
Risk-based processes to prevent workforce infections that:
- Ensures practices align with relevant state or territory work health and safety regulations, as well as the current edition of the Australian Guidelines for the Prevention and Control of Infection in Healthcare.
- Complies with state and territory public health requirements for workforce screening and designated exclusion periods.
- Develops strategies to manage infection risks affecting the workforce, patients, and consumers, including those related to novel infections.
- Encourages staff and volunteers to abstain from work or visiting healthcare settings when infection is suspected or confirmed.
- Tracks and regulates the flow of healthcare staff between clinical areas, care settings, amenity areas, and different health service organisations.
- Provides guidelines and resources for workforce members who are required to isolate or quarantine following exposure to or acquisition of an infection.
- Establishes systems for the monitoring, investigation, and management of infection outbreaks.
- Formulates plans to maintain ongoing service provision during outbreaks, pandemics, or events with increased infection transmission risks.
Action 3.18: Antimicrobial stewardship program
Developing a program that:
- Integrate a comprehensive antimicrobial stewardship policy into the organisation's infection prevention strategy.
- Offer access to current, evidence-based Australian therapeutic guidelines for antimicrobial prescribing, and promote their utilisation.
- Maintain an antimicrobial formulary that aligns with current evidence-based Australian therapeutic guidelines, complete with restriction rules and approval processes.
- Implement core components, recommendations, and principles from the prevailing Antimicrobial Stewardship Clinical Care Standard.
- Use the outcomes of audits on antimicrobial usage and appropriateness as a basis for ongoing quality improvement.
Action 3.19: Applying the antimicrobial stewardship program:
Organisations should ensure the program will:
- Periodically examine the patterns of antimicrobial prescribing and usage within the organisation.
- Leverage surveillance data concerning antimicrobial resistance to inform and improve appropriate prescribing practices.
- Assess the efficacy of the program, pinpoint areas needing enhancement, and initiate actions to better the appropriateness of antimicrobial prescribing and usage.
- Report to clinicians and governing bodies by:
- Delivering regular reports on compliance with the antimicrobial stewardship policy and guidelines.
- Highlighting areas requiring targeted interventions to combat antimicrobial resistance.
- Monitoring and reporting the organisation’s longitudinal performance related to the use and appropriateness of antimicrobials.
National Safety and Quality Health Service (NSQHS) Standards
Failure to comply with the requirements could lead to an organisation being penalised or reprimanded.
Related Training Requirements
The following Training Requirement guides can be used to support and facilitate the NSQHS infection prevention and control training requirement
Infection Prevention Skills Staff Need for NSQHS Compliance
Healthcare staff need a diverse set of skills to comply fully with the NSQHS standards on infection prevention. The following elaborates on the essential skills required:
| Skill | Key Elements |
|---|---|
| Understanding of Infection Types and Transmission Mechanisms |
Staff should be well-versed in different types of infections like bacterial, viral, and fungal, as well as their modes of transmission, including airborne, droplet, and contact transmission. This understanding is critical for implementing targeted infection control measures. |
| Competence in Hand Hygiene Techniques |
Effective hand hygiene is a cornerstone of infection control. Staff should be proficient in the 'Five Moments for Hand Hygiene' outlined by the World Health Organisation. This includes the critical times when hand hygiene should be performed, such as before patient contact and after touching patient surroundings. |
| Knowledge of Proper Use and Disposal of PPE |
Personal protective equipment (PPE) like masks, gloves, and gowns serve as barriers to infection. Staff should know not just how to wear PPE, but also how to safely remove and dispose of it to prevent cross-contamination. |
| Environmental Cleaning Skills |
The ability to adequately clean and disinfect patient and procedure rooms is essential. This includes knowledge of which cleaning agents to use and understanding the frequency and extent of cleaning required. |
| Ability to Conduct and Interpret Infection Control Audits |
Routine audits can reveal gaps in infection control measures. Staff should know how to conduct these audits, collect and interpret data, and make informed decisions for quality improvement. |
| Communication Skills |
Effective communication is key to infection control. Staff must be able to clearly instruct patients on infection prevention measures and articulate concerns or observations to their colleagues. |
| Knowledge of Infectious Diseases Legislation and Guidelines |
Familiarity with regulations set by the Aged Care Quality and Safety Commission and the Australian Commission on Safety and Quality in Health is essential for compliance. |
| Ability to Report and Manage Infection Incidents |
Accurate reporting is crucial for quality improvement and incident management. Staff should be able to document infection incidents comprehensively and understand the reporting chain within their organisation. |
How to Assess Staff Competency in Infection Prevention
Effective assessment strategies are integral to ensuring that staff are competent in infection prevention. These may include:
- Self-Assessments: Questionnaires that staff can fill out to assess their own understanding.
- On-The-Job Observations: Supervisors can observe staff during their shifts to assess their practical skills.
- Audits: Regular audits can provide valuable data on compliance levels.
- Simulation Exercises: Simulated infection scenarios can offer a practical, hands-on method for assessment.
Strategies to Support Healthcare Staff Improve Infection Prevention Skills for the NSQHS standard
Developing and maintaining staff skills in infection prevention can be achieved through a variety of strategies:
- Regular Training Sessions: Routine workshops to refresh and update skills.
- Workshops and Seminars: In-depth sessions on specific aspects of infection control.
- Online Modules: Online courses can be a flexible option for skill development.
- On-the-Job Training: Practical experience under supervision offers invaluable learning opportunities.
Sample Training Plan for the Infection Prevention (NSQHS) Training Requirement
Ensuring staff are competent in the relevant skills is pivotal to facilitate best-practice infection prevention and control.
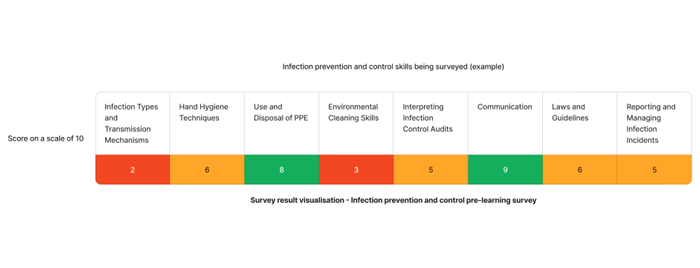
Using the above survey as an example - The skills that requires the most attention are infection types and transmission mechanisms and environmental cleaning skills. We can target learning initiatives to fill these gaps to enhance staff competency.
| Quarter | Topics | Resources |
|---|---|---|
| Q1 | Infection Types and Transmission Mechanisms |
|
| Q2 | Environment Cleaning Skills |
Need an LMS that can support infection prevention learning?
Contact Ausmed today and see how we can support with your infection prevention and control requirements!
Staff Competency Assessment for Infection Prevention (NSQHS Standards) - Example
The following is an example survey that learning and development coordinators may use to asses staff competency on clinical assessment.
Staff Survey - Infection Prevention Competency
-
How often should hand hygiene be performed?
- [Answer here]
-
What are the types of PPE used in your workplace?
- [Answer here]
-
How is waste segregation conducted in your unit?
- [Answer here]
-
What is the procedure for a needlestick injury?
- [Answer here]
-
How often are infection control audits conducted?
- [Answer here]
-
Are you familiar with the infection prevention guidelines from the Aged Care Quality and Safety Commission?
- Yes
- Somewhat
- No
Conclusion
Infection prevention is not only a regulatory requirement but also a moral obligation for healthcare organisations. A well-rounded, ongoing training program can play a crucial role in ensuring that healthcare providers are equipped with the skills and knowledge to prevent healthcare-associated infections effectively.
References
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Preventing and Controlling Infections Standard'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.05'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.06'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.07'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.08'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.09'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.13'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.14'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.15'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.16'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.18'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 3.19'
- Australian Commission on Safety and Quality in Health, 2023. Australian Guidelines for the Prevention and Control of Infection in Healthcare
- Australian Government Department of Health and Aged Care, 2023. Australian Immunisation Handbook
- Australian Commission on Safety and Quality in Health, 2023. Antimicrobial Stewardship Clinical Care Standard