A Core Component of Governance and Safe Care
Measurement and Quality Improvement (MQI) systems are essential for providing safe, high-quality aged care and healthcare. These systems support services in monitoring performance, analysing outcomes, and implementing changes that improve people's safety, experience, and wellbeing.
This Training Requirement briefly outlines the expectations for establishing and maintaining quality systems and helps organisations translate those into action across governance, operations, and the workforce.
Read our article: Action 2.9.5 – What is an Effective Training System? for guidance on how training systems can support quality and compliance initiatives like this one.
Using this Training Requirement
This resource outlines the specific requirements for Measurement and Quality Improvement in the:
- NSQHS Standards (Actions 1.08 & 1.09)
- Strengthened Aged Care Quality Standards (2025) – particularly Outcome 2.2 and Outcome 2.3
It explains:
- Key regulatory actions
- What systems and responsibilities are needed
- When education or training is required
- What evidence may be asked for during an assessment
National Aged Care Mandatory Quality Indicator Program
Note: This guide does not explicitly cover the National Aged Care Mandatory Quality Indicator Program in detail. For a comprehensive overview of the program and recent updates, refer to our article: Overview of the National Aged Care Mandatory Quality Indicator Program.
Understanding the Relevant Actions in the Standards
NSQHS Standards
Action 1.08 – Quality Improvement Systems
The organisation must:
- Identify safety and quality measures and monitor performance
- Use data to identify improvement opportunities
- Implement and evaluate improvement strategies
- Engage consumers and staff in the improvement process
Action 1.09 – Reporting Performance
The organisation must provide timely reports on safety and quality to the governing body, workforce, consumers, and others.
Strengthened Aged Care Quality Standards
Outcome 2.2 – Quality, Safety and Inclusion Culture
- Action 2.2.1: The governing body leads a culture of continuous improvement and quality care
- Action 2.2.2: The organisation ensures that safety, health and inclusion are embedded into strategic and operational planning
Outcome 2.3 – Accountability and Quality System
The provider must implement a quality system that:
- Uses data (e.g. risks, incidents, feedback, quality indicators) to monitor and improve performance
- Regularly reviews system effectiveness and reports results to older people, workers and governance
- Demonstrates continuous improvement and open disclosure when things go wrong
Accountability for Quality Improvement
Governing Body Accountability
The governing body must set strategic priorities, lead a culture of improvement, and oversee the effectiveness of the organisation’s quality system. It is also responsible for using data, QI results, and feedback to inform decision-making.
Operational Accountability
Operational leads (Quality, Clinical Governance, HR, and Operations) are responsible for:
- Implementing QI strategies
- Monitoring performance against key indicators
- Analysing incidents and feedback
- Reporting and escalating risks and improvement priorities
Workforce Roles
Staff across all levels contribute to measurement and improvement by:
- Participating in data collection and reporting
- Escalating issues
- Supporting or leading improvement projects
- Using feedback to inform their daily practice
Meeting Measurement and Quality Improvement Requirements
To meet the standards, organisations should implement a structured and transparent quality system with these components:
1. Quality System Framework
- Policies and procedures for QI planning and reporting
- A quality plan that aligns with strategic goals
- Clear roles and accountabilities for quality activities
2. Use of Data for Monitoring and Reporting
- Identify relevant measures for care quality and workforce capability
- Monitor incidents, feedback, complaints, and QI data
- Report findings to governance, workers, and consumers
- Use National Quality Indicator Program data to drive improvement
3. Consumer and Workforce Engagement
- Involve staff and older people in identifying improvement opportunities
- Share results and priorities with consumers in accessible ways
- Establish advisory or working groups to support improvement projects
4. System Review and Continuous Improvement
- Conduct audits and reviews of the QI system’s effectiveness
- Track outcomes of improvement initiatives
- Use QI data to inform service planning and risk management
5. Training and Education (If Required)
Training may be needed when:
- Staff contribute to quality data collection or improvement initiatives
- Managers are responsible for reporting and improvement cycles
- Governance or leadership require upskilling on performance monitoring or regulatory requirements
Training topics may include:
- Principles of continuous improvement
- Using QI tools (e.g. PDSA cycles, root cause analysis)
- Analysing feedback and incident data
- Interpreting and using QI performance reports
Use Quality Data to Inform Education
Training should be guided by evidence. Quality and safety data, particularly findings from incidents, audits, complaints, and Quality Indicator Program results, should be used to validate when and for whom education is required. This avoids generic or ineffective “spray-and-pray” training and ensures education addresses the actual cause or performance gap.
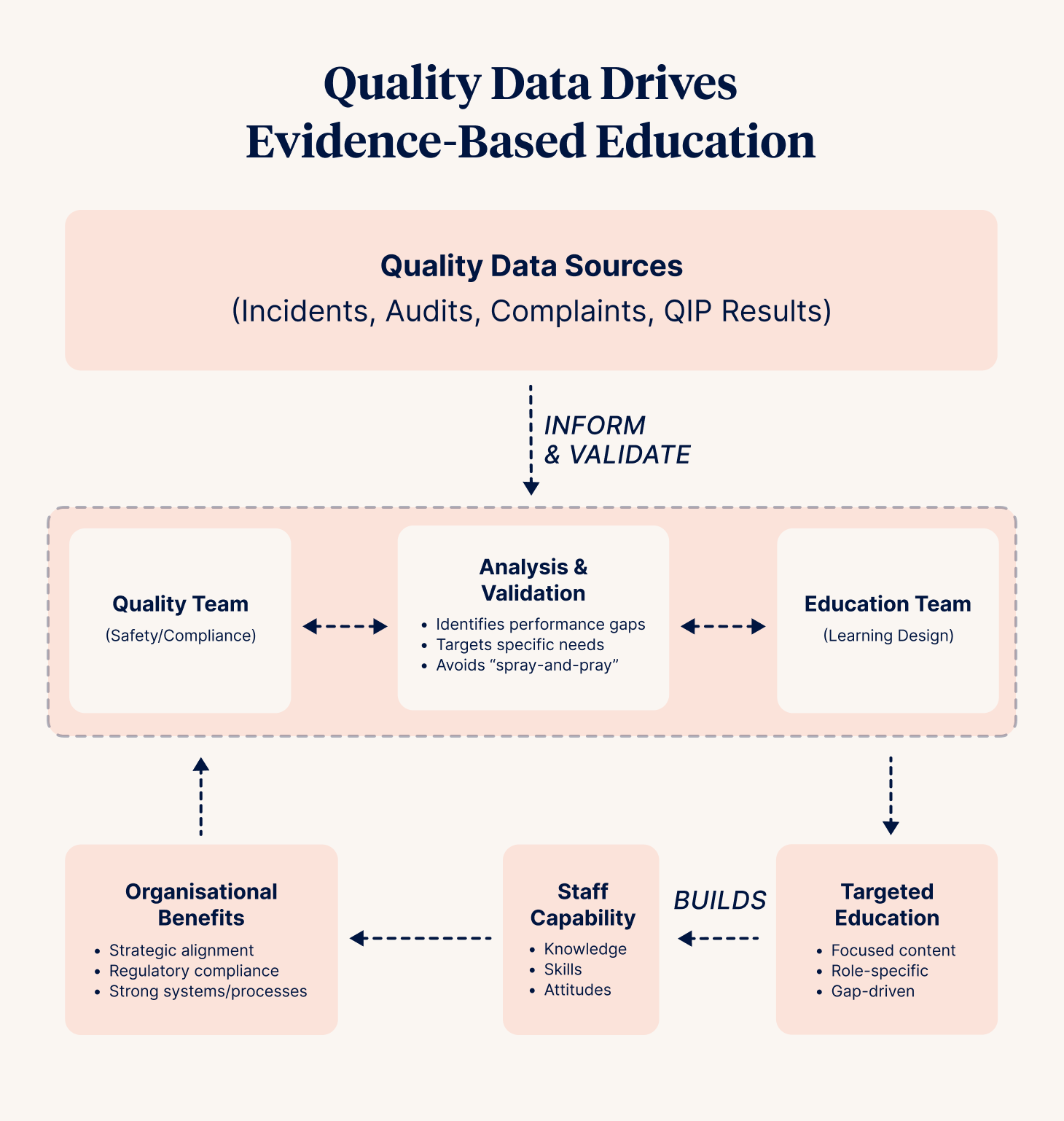
Aligning Quality and Education Frameworks
Integrating clinical education and quality initiatives has strategic, regulatory, and operational benefits. When learning and quality teams collaborate, they not only support compliance but also build strong internal systems and processes that grow staff knowledge, skills, and capability across the organisation.
Education Is Not Always the Solution!
Training is only one part of a quality improvement approach. It should not be a default solution for broader system failures, process gaps, or unclear expectations. Instead, a structured review of root causes should guide the response, whether redesigning workflows, improving supervision, updating policies, or delivering targeted education.
Evidence of Compliance
Organisations can demonstrate a robust and effective approach to policy and procedure management by referring to detailed lists of evidence that may be audited:
- Strengthened Aged Care Quality Standards Evidence Mapping Framework (the auditor's tool)
- NSQHS Standards Action 1.07 Strategies for improvement
The following items are identified as items auditors may request to assess the effectiveness of your quality system:
| Requirement | Evidence Examples |
|---|---|
| Quality System | Quality plans, QI policies, governance oversight |
| Measurement and Monitoring | Dashboards, audit reports, incident trend analysis, and feedback reports |
| Engagement | Minutes from consumer or staff quality forums, evidence of co-designed improvements |
| QI Reviews and Actions | Records of system reviews, documented improvements, and lessons learned |
| Training Records | Records of training in QI systems or methods, governance onboarding for monitoring responsibilities |
| Quality Indicator Program | QI submissions, internal QI data reports, and improvement actions linked to QI data |
Ensure your organisation is prepared for your first audit under the strengthened Standards.
Quality is Everyone’s Business
Measurement and quality improvement are not just compliance tasks. They are strategic enablers of safer, better care. They support continuous improvement, informed decision-making, and shared accountability. When embedded into governance, operations, and workforce practices
Training plays a role, but should be driven by data and not used as a default solution to systemic issues. Aligning quality and education systems ensures capability-building is targeted, effective, and supports meaningful change.



