In an ideal world, we’d be able to diagnose and treat patients without any harmful side effects. Medical imaging remains one of the best ways to achieve this, as it allows us to see what’s going on inside the body without the need for surgery or other invasive procedures. Indeed, it’s something we’re perhaps guilty of taking for granted at times.
Medical imaging can be used for both diagnosis and therapeutic purposes, making it one of the most powerful resources available to effectively care for our patients.
In terms of diagnosis, common imaging types include:
- CT (computer tomography)
- MRI (magnetic resonance imaging)
- Ultrasound
- X-ray
- Nuclear medicine imaging (including positron emission tomography (PET)).
Each type works slightly differently to create images of what’s going on inside the body. Let’s look at them a little closer.
Ultrasound

Ultrasound is a typically non-invasive and safe form of medical imaging that has a wide range of applications (NPS MedicineWise 2019).
Ultrasound uses sound waves rather than ionising radiation. High-frequency sound waves are transmitted from a probe to the body via conducting gel. Those waves then bounce back when they hit the different structures within the body, creating a real-time image (FDA 2024).
Another type of ultrasound commonly used is the ‘Doppler’, which allows the blood flow through the arteries and veins to be visualised (FDA 2024).
Due to the minimal risk associated with ultrasound imaging, it’s the first choice for viewing the fetus during pregnancy (FDA 2024). However, as its applications are so wide, it tends to be the first port of call for many patients. Ultrasound imaging can be used to diagnose conditions in other areas of the body, including the:
- Abdomen
- Pelvis
- Blood vessels
- Breasts
- Kidneys
- Muscles
- Bones
- Joints.
(Healthdirect 2024a; FDA 2024)
X-Ray Imaging

X-ray imaging is one of the oldest but most frequently used imaging types (Cleveland Clinic 2024).
Discovered in 1895, X-rays are a form of electromagnetic radiation. They work on a wavelength and frequency that we’re unable to see with the naked human eye. However, they can penetrate through the skin to create a picture of what’s going on beneath (History.com 2025).
While typically used to diagnose issues affecting the skeletal system, X-rays can also detect other issues, such as breast cancer (through mammography) and digestive issues (through barium swallows and enemas) (FDA 2023a; Better Health Channel 2019).
X-rays are widely used as they are quick and relatively easy for the patient to endure. However, there are risks associated with the use of radiation for X-ray imaging.
Every time a patient undergoes an X-ray, they receive a dose of ionising radiation. This may go on to cause issues such as:
- Slightly increased risk of cancer later in life
- Cataracts
- Skin reddening
- Hair loss
- Disturbance in the growth of a fetus in a pregnant patient
- A reaction to intravenously injected contrast agents or dyes that are used to assist with visualisation.
(FDA 2023a)
Most of these risks are mitigated by only using X-rays when strictly necessary, and correctly shielding the patient's body.
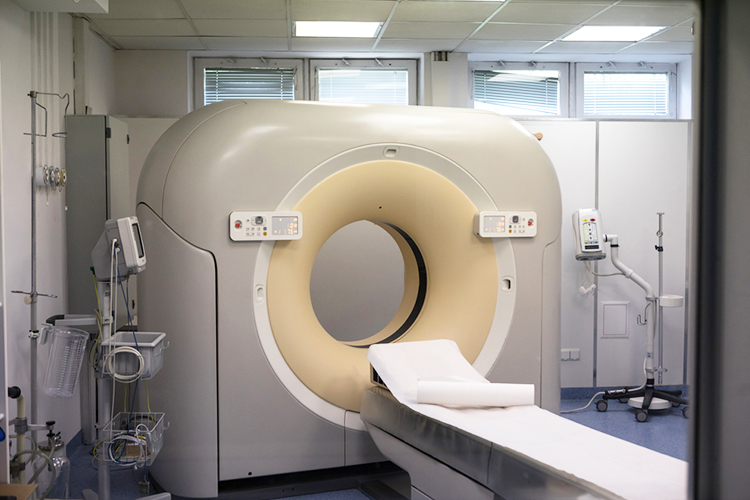
Computer Tomography (CT)

Computer tomography (CT) (also known as computed axial tomography (CAT)) uses X-rays to produce cross-sectional images of the body (NPS MedicineWise 2019). The CT scanner has a large circular opening so that the patient can lie on a motorised table. An X-ray source and a detector then rotate around the patient, producing a narrow ‘fan-shaped’ beam of X-rays. These X-rays pass through sections of the patient’s body in order to create 'snapshots', which are then collated into one or multiple images of the internal organs and issues (FDA 2023b).
CT scans provide greater clarity than conventional X-rays, producing more detailed images of the internal organs, bones, soft tissue and blood vessels within the body (FDA 2023b).
The benefits of using CT scans far exceed the risks, which (like with X-rays) include an increased risk of cancer, harm to an unborn child or a reaction to the contrast agent or dye used. In many cases, the use of a CT scan prevents the need for exploratory surgery (FDA 2023b).
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging (MRI) creates diagnostic images without using harmful radiation (NPS MedicineWise 2019).
MRI uses a strong magnetic field and radio waves to generate detailed images of organs, soft tissues, bones, ligaments and cartilage (NPS MedicineWise 2019). It is commonly used to examine internal body structures in order to assess:
- Brain and spinal cord abnormalities
- Breast, prostate, liver and other abnormalities
- Joint abnormalities or injuries
- Spinal injuries
- Tendon and ligament tears
- Heart structure and function
- Areas of activation in the brain
- Blood flow through blood vessels and arteries
- Chemical composition of tissues
- Organs in the pelvis, chest and abdomen (e.g. heart, liver, kidney, spleen).
(FDA 2018; MITA 2020)
As we know, the human body is mostly made of water, and each water molecule contains a hydrogen nucleus (proton). An MRI scanner uses a strong magnetic field to force the protons to align with that field. A radio frequency is then applied, which stimulates the protons and spins them out of equilibrium. When the frequency is turned off, the protons return to their original alignment, releasing energy that is detected by the MRI sensors (NIBIB n.d.).
Protons in different body tissues return to their normal alignment at different rates, allowing the MRI to distinguish between various types of tissue and identify any abnormalities. The way in which the molecules ‘flip’ and return to their normal spin alignment is recorded and processed into an image (NIBIB n.d.).
MRI doesn’t use harmful ionising radiation. However, there are other disadvantages associated with its use.
As strong magnets are used, metal implants such as pacemakers and implantable cardioverter-defibrillators (ICDs) in the patient's body may be hazardous as they may be moved or heated up within the magnetic field (Cleveland Clinic 2021). There have been several reported cases of patients with pacemakers dying through the use of MRI (Nordbeck et al. 2015). Other disadvantages associated with MRI include:
- The loud noise from the scanner, which necessitates the need for ear protection
- Length of the procedure
- Magnetic objects being attracted to the strong magnetic field and potentially becoming dangerous projectiles (for this reason, objects entering the magnetic field must be screened carefully)
- Heating of the body
- Adverse reactions to the contrast agent
- Potential feelings of claustrophobia
- The need to remain still for the duration of the procedure (potentially requiring patients to be sedated).
(FDA 2018; NPS MedicineWise 2019)
Positron Emission Tomography (PET)

A positron emission tomography (PET) scan involves injecting, swallowing or inhaling a radioactive agent known as tracer. The patient then lies in a PET scanner, a large doughnut-like structure that detects gamma rays from the tracer and converts them into images. Bright spots on the image indicate higher chemical activity, potentially caused by a disease (Healthdirect 2024b).
PET scans are used to diagnose conditions such as tumours, heart disease and brain disorders. They can be used to assess the entire body or one specific area (Healthdirect 2024b).
While PET scans are generally painless for the patient, they involve exposure to ionising radiation. Other disadvantages include the risk of adverse reactions to the radioactive material and potential feelings of claustrophobia for the patient (NPS MedicineWise 2019).
Conclusion
One thing we do have to be aware of as medical professionals in a time of escalating medical costs and increasing demand is that we’re using the best resources available to meet the needs of our patients. This means making a careful decision about the right medical imaging for each patient and their potential diagnosis.
Test Your Knowledge
Question 1 of 3
What is a primary reason ultrasound is often the first imaging choice during pregnancy?
Topics
References
- Better Health Channel 2019, Barium Tests, Better Health Channel, viewed 14 April 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/barium-tests
- Cleveland Clinic 2021, Are MRI Scans Safe If You Have a Pacemaker or Implanted Device?, Cleveland Clinic, viewed 14 April 2025, https://health.clevelandclinic.org/are-mri-scans-safe-if-you-have-a-pacemaker-or-implanted-device
- Cleveland Clinic 2024, X-Ray, Cleveland Clinic, viewed 14 April 2025, https://my.clevelandclinic.org/health/diagnostics/21818-x-ray
- Healthdirect 2024a, Ultrasound, Australian Government, viewed 14 April 2025, https://www.healthdirect.gov.au/ultrasound
- Healthdirect 2024b, PET Scan, Australian Government, viewed 14 April 2025, https://www.healthdirect.gov.au/pet-scan
- History.com 2020, German Scientist Discovers X-rays, A&E Television Networks, viewed 14 April 2025, https://www.history.com/this-day-in-history/german-scientist-discovers-x-rays
- The Medical Imaging & Technology Alliance 2020, Magnetic Resonance Imaging (MRI), National Electrical Manufacturers Association, viewed 14 April 2025, https://www.medicalimaging.org/about-mita/modalities/magnetic-resonance-imaging-(mri)
- National Institute of Biomedical Imaging and Bioengineering n.d., Magnetic Resonance Imaging (MRI), National Institutes of Health, viewed 14 April 2025, https://www.nibib.nih.gov/science-education/science-topics/magnetic-resonance-imaging-mri
- Nordbeck, P, Ertl, G & Ritter, O 2015, ‘Magnetic Resonance Imaging Safety in Pacemaker and Implantable Cardioverter Defibrillator Patients: How Far Have we Come?’, European Heart Journal, vol. 36, no. 24, viewed 14 April 2025, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4475571/
- NPS MedicineWise 2019, Imaging Explained, NPS MedicineWise, viewed 14 April 2025, https://www.nps.org.au/consumers/imaging-explained
- U.S. Food & Drug Administration 2017, MRI (Magnetic Resonance Imaging), United States Government, viewed 14 April 2025, https://www.fda.gov/radiation-emitting-products/medical-imaging/mri-magnetic-resonance-imaging
- U.S. Food & Drug Administration 2023a, Medical X-ray Imaging, United States Government, viewed 14 April 2025, https://www.fda.gov/radiation-emitting-products/medical-imaging/medical-x-ray-imaging
- U.S. Food & Drug Administration 2023b, Computed Tomography (CT), United States Government, viewed 14 April 2025, https://www.fda.gov/radiation-emitting-products/medical-x-ray-imaging/computed-tomography-ct
- U.S. Food & Drug Administration 2024, Ultrasound Imaging, United States Government, viewed 14 April 2025, https://www.fda.gov/radiation-emitting-products/medical-imaging/ultrasound-imaging