Earache (otalgia) is the term used to describe feelings of discomfort, including pain, pressure or blockage, in one or both ears.
Otalgia can be classified as either:
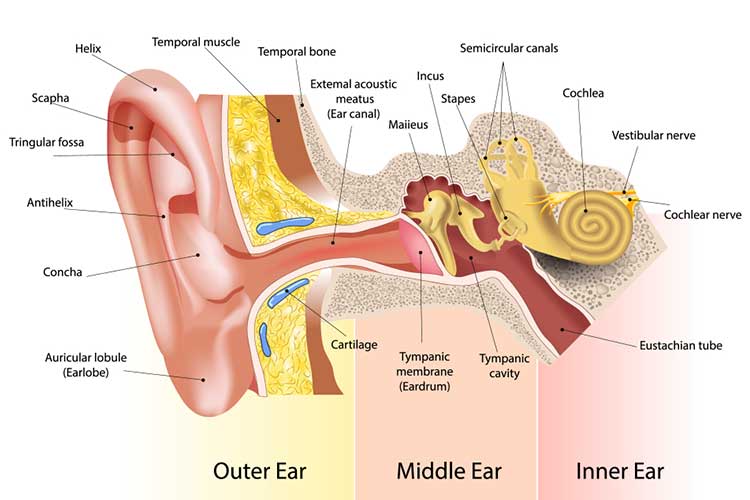
- Primary otalgia: Pain that arises directly from the inner, middle or external ear
- Secondary otalgia (also known as referred otalgia): Pain caused by an issue in another area of the body that shares the same nerves as the ear.
(Coulter et al. 2024; Kaylie 2022)
The most common reason for ear-related otalgia is a blockage of the passageway between the middle ear and the back of the throat. This passage is known as the Eustachian tube (LeWine 2023).
Most otalgia resolves within a few days. Even in the case of prolonged ear infections, the prognosis is usually favourable (Havard Health Publishing 2019).
Note: this article is intended to provide an overview of otalgia in adults.
Causes of Otalgia
Otalgia has a variety of causes, including but not limited to:
Primary Otalgia
- Infection e.g. acute otitis media, chronic suppurative otitis media
- Foreign body in the ear
- Injury
- Neoplasm
- Ear wax build-up
- Inflammation.
Secondary Otalgia
- Dental problems
- Issues with the jaw.
(Coulter et al. 2024; Mendis 2023)
Symptoms of Otalgia
Otalgia is most commonly associated with a feeling of obstruction or blockage in the ear. It may begin gradually or suddenly, and the pain may feel very intense (LeWine 2023).
Often, otalgia will clear up after a few days without intervention. If it doesn’t, however, it’s wise to see a general practitioner (GP).
Patients should be advised to seek help if they:
- Experience symptoms for more than three days
- Are feeling generally unwell
- Have a fever
- Are experiencing discharge leaking from the ear
- Are experiencing worsening hearing
- Have an obstruction in their ear.
(Healthdirect 2024)
Clear or bloody fluid accompanied by severe ear pain may signal a ruptured eardrum. A ruptured eardrum is a hole or perforation in the membrane that separates the inner or outer ear (Mount Sinai 2024).
If the eardrum ruptures because of a middle ear infection, the pain often decreases because the pressure is reduced (LeWine 2023).
A ruptured eardrum can be caused by injury to the ear, changes in air or water pressure (for example, from diving), ear infections, foreign objects in the ear or as a result of very loud noises (Mount Sinai 2024).
If chronic pain is accompanied by a ringing or buzzing sound, it may be tinnitus (Healthdirect 2023).

Diagnosing Otalgia
If otalgia is severe and/or if other symptoms are present, it’s recommended that the person seek out advice from a health professional.
Usually, a GP will examine the ears, nose and throat of a person with otalgia. This will be carried out with an otoscope to look inside the ears and investigate redness and fluid buildup. The GP may also test for any hearing loss (LeWine 2023).

Treating Otalgia
If pain is caused by a blocked Eustachian tube, a decongestant or antihistamine may help relieve it (LeWine 2023).
Until the underlying problem is treated or cleared up, pain-relief medicines will usually be enough to control the pain (LeWine 2023).
Non-medicinal methods of easing the pain include holding a warm cloth or heat pack to the ear and resting the head on two or more pillows when sleeping (Healthdirect 2024).
If symptoms last for more than three days or discharge is leaking from the ear, antibiotics may be prescribed (Healthdirect 2024).
If a patient is concerned or believes medication is required for the otalgia, they should seek information from a doctor and/or pharmacist.
Preventing Otalgia

The following is advised for preventing otalgia:
- Avoiding allergy triggers
- Practising ear hygiene
- Wearing ear protection when needed (e.g. when exposed to loud noise)
- Wearing earplugs and a swimming cap while swimming
- Preventing water from getting into the ear
- Keeping all foreign objects out of the ear.
(Coulter et al. 2024; Healthdirect 2024)
Test Your Knowledge
Question 1 of 3
Which one of the following is a potential cause of secondary otalgia?
Topics
Further your knowledge
References
- Coulter, J, Hohman, MH & Kwon, E 2024, ‘Otalgia’, StatPearls, viewed 2 December 2024, https://www.ncbi.nlm.nih.gov/books/NBK549830/
- LeWine, HE 2023, Earache, Harvard Medical School, viewed 2 December 2024, https://www.health.harvard.edu/a_to_z/earache-a-to-z
- Healthdirect 2024, Earache, Australian Government, viewed 2 December 2024, https://www.healthdirect.gov.au/earache
- Kaylie, DM 2022, Earache, MSD Manual, viewed 2 December 2024, https://www.msdmanuals.com/en-au/home/ear,-nose,-and-throat-disorders/symptoms-of-ear-disorders/earache
- Masters, M 2023, What Is Ear Pain? Symptoms, Causes, Diagnosis, Treatment, and Prevention, Everyday Health, viewed 2 December 2024, https://www.everydayhealth.com/ear-pain/guide/
- Mendis, S 2023, Otalgia, Patient, viewed 2 December 2024, https://patient.info/doctor/otalgia-earache
- Mount Sinai 2024, Ruptured Eardrum, Mount Sinai, viewed 2 December 2024, https://www.mountsinai.org/health-library/diseases-conditions/ruptured-eardrum