Despite seeming like minor injuries, skin tears can be complex wounds with the potential to significantly affect a patient’s health and cause chronic discomfort (LeBlanc n.d.).
Skin tears are often misdiagnosed and underreported, and in many cases, are preventable (LeBlanc et al. 2018).
What are Skin Tears?
The International Skin Tear Advisory Panel defines a skin tear as:
‘A traumatic wound caused by mechanical forces, including removal of adhesives. Severity may vary by depth (not extending through the subcutaneous layer).’
(LeBlanc et al. 2018)
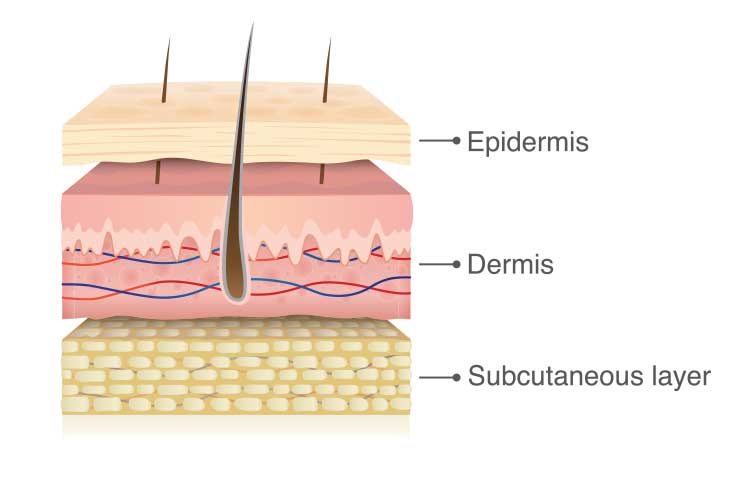
Skin tears are acute, traumatic injuries caused by shearing, friction or blunt force wherein the layers of skin are separated. This may be a separation of the epidermis from the dermis (partial thickness) or separation of both the epidermis and dermis from underlying structures (full thickness) (LeBlanc et al. 2018).
Any part of the body can be affected by skin tears, but 70 to 80% of tears occur on the arms and hands (LeBlanc et al. 2018).
Skin tears most commonly affect those with fragile skin, particularly older people (LeBlanc et al. 2018).
Why are Older People More Susceptible to Skin Tears?
The physiology of skin undergoes several changes with age, causing it to become more fragile and vulnerable to trauma:
- The epidermis thins
- The epidermal junction flattens
- There is a loss of collagen, elastin and glycosaminoglycans
- Levels of dermal proteins (which contain moisture) decrease
- The dermis will atrophy and contract
- There is decreased activity of sweat glands and sebaceous glands
- Blood vessel walls thin, and blood supply to the extremities decreases.
(LeBlanc et al. 2018)
These changes, in tandem with reduced skin regeneration abilities and a weakened protective immune system, mean that an older person’s skin integrity can be damaged by even a small amount of force (LeBlanc et al. 2018).
Risk Factors for Skin Tears
Factors that increase the risk of developing skin tears include:
- Older age
- Dry and fragile skin
- Previous skin tears
- Taking medications that cause skin thinning (e.g. steroids, immunosuppressants, anti-inflammatories, anticoagulants)
- Impaired mobility
- Limited dexterity, which can interfere with washing or drying the skin
- Visual impairment
- Sensory or cognitive impairment
- Comorbidity (e.g. chronic heart disease, diabetes, renal failure, stroke)
- Dehydration
- Poor nutrition
- Swallowing or dental issues, which can lead to poor nutrition
- Radiation therapy.
(LeBlanc n.d.; VIC DoH 2024a)
Preventing Skin Tears

Identifying at-risk patients through a holistic skin assessment on admission is crucial in preventing skin tears (LeBlanc et al. 2018).
The healthcare worker should assess:
- The patient’s skin
- The patient’s medical history
- Intrinsic risk factors for vulnerable skin
- Whether the skin is intact
- Wound-related risk factors (e.g. eczema, oedema)
- Any skin conditions, rashes, itches, pain or other unusual issues
- The patient’s knowledge about the condition of their own skin
- History of skin conditions
- Physical factors (temperature, texture).
(Beeckman et al. 2020)
A risk reduction program checklist should be implemented for patients deemed at-risk. See: Best Practice Recommendations for Holistic Strategies to Promote and Maintain Skin Integrity (p. 13).
When caring for patients at risk of experiencing skin tears, healthcare workers should take the following measures:
- Keeping fingernails short
- Not wearing jewellery
- Padding or removing dangerous furniture or devices (e.g. bed rails, wheelchairs)
- Covering the skin of vulnerable patients with appropriate clothing, shin guards or retention bandages/stockinettes
- Using products that are pH balanced and have preventative emollients to maintain the patient’s skin integrity
- Reducing the patient’s sun exposure
- Minimising the frequency of the patient’s bathing, ensuring water is not too hot and gently patting their skin dry with a soft towel (instead of rubbing)
- Regular moisturising.
(LeBlanc et al. 2018; Beeckman et al. 2020)
Identifying and Assessing Skin Tears
Correct and prompt identification of skin tears is essential in the effective management of the wound. A thorough examination of the skin tear as well as a holistic patient assessment (see above) should be performed upon presentation (LeBlanc et al. 2018).
The following should be documented as part of the skin tear assessment:
- Cause of the skin tear
- Anatomical location and duration
- Dimensions (length, width, depth)
- Wound bed characteristics
- Percentage of viable and non-viable tissue
- Exudate (type and amount)
- Any bleeding or haematoma
- Integrity of the surrounding skin
- Any signs or symptoms of an infection
- Any pain related to the wound.
(LeBlanc et al. 2018)
The main tools used to classify skin tears include the Skin Tear Audit Research (STAR) classification system and the International Skin Tear Advisory Panel (ISTAP) classification system.
The Skin Tear Audit Research (STAR) classification system
| Category | Edges | Colour of skin or flap |
| 1A | Edges can be realigned to their normal anatomical position (without excessive stretching). | Not pale, dusky or darkened. |
| 1B | Edges can be realigned to their normal anatomical position (without excessive stretching). | Pale, dusky or darkened. |
| 2A | Edges can not be realigned to their normal anatomical position (without excessive stretching). | Not pale, dusky or darkened. |
| 2B | Edges can not be realigned to their normal anatomical position (without excessive stretching). | Pale, dusky or darkened. |
| 3 | The skin flap is completely absent. |
(Adapted from VIC DoH 2024b)
The International Skin Tear Advisory Panel (ISTAP) classification system
| Category | Description |
|---|---|
| Type 1: No skin loss | Linear or flap tear which can be repositioned to cover the wound bed. |
| Type 2: Partial flap loss | Partial flap loss which cannot be repositioned to cover the wound bed. |
| Type 3: Total flap loss | Total flap loss exposing entire wound bed. |
(Adapted from ISTAP 2020)
Managing Skin Tears
Prompt and appropriate treatment of skin tears improves patient outcomes. The goals of treatment are primarily to:
- Preserve the skin flap
- Protect the surrounding tissue
- Re-approximate the edges of the wound (without excessive stretching)
- Reduce the risk of further infection or injury.
(LeBlanc et al. 2018)
The process of treating skin tears is as follows:
1. Control any bleeding.
- Apply pressure to the wound.
- Elevate the affected limb if possible.
2. Cleanse the wound.
- Remove residual debris or haematoma with a non-woven swab.
- Cleanse the wound with warm, sterile isotonic saline (sodium chloride 0.9%) or water.
- Gently pat the surrounding skin dry; the wound itself should be left to air dry.
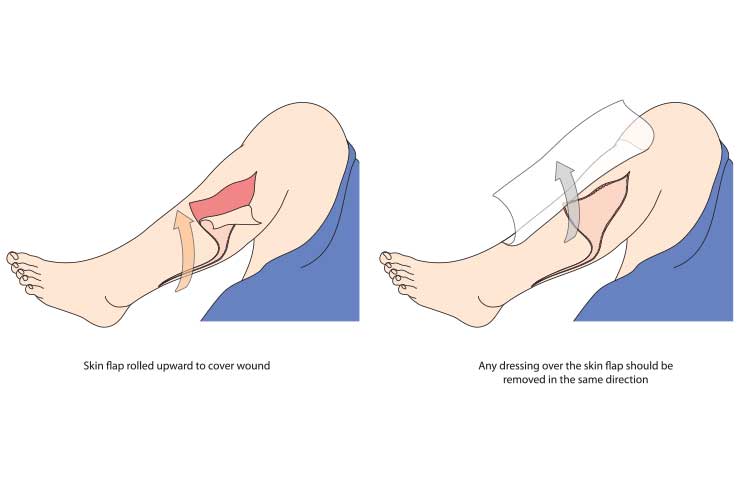
3. Approximate the skin flap.
- If the skin flap is viable (category 1 or 2), gently ease it back into place to use as a dressing (using a gloved finger, dampened cotton tip, tweezers or silicone strip).
- If this is difficult, rehydrate the flap using a moistened non-woven swab for 5-10 minutes.
- Do not excessively stretch the flap during approximation.
- If the skin flap is non-viable or necrotic, it should be debrided. Ensure this is performed by an experienced nurse.
4. Dress the wound.
- An appropriate non-adherent dressing should be chosen depending on the wound characteristics and classification. The chosen dressing should:
- Maintain a moist healing environment
- Protect the wound and surrounding skin from further trauma and dressing removal
- Manage any exudate and/or infection
- Be easy to apply
- Be able to stay in situ for a long period of time
- Be cost-effective.
- Apply the dressing, securing it with a non-adhesive silicone-interfaced dressing material (e.g. arm/leg protector, flexible netting).
- Mark the dressing with an intended removal date and an arrow indicating the removal direction.
- Films and tapes should not be used on fragile skin.
5. Monitoring and Reassessment
- Leave the initial dressing in situ for no longer than five days.
- If the skin flap is pale, dusky or darkened, it should be reassessed within 24 to 48 hours.
- The wound should be monitored for any infections or changes. If infection or exudate is present, the dressings should be changed more frequently.
- If there is no sign of infection or deterioration after the initial dressing, subsequent dressings should be left in situ for about five days.
- If there is no improvement after four reassessments, refer the patient to a specialist.
(LeBlanc et al. 2018; VIC DoH 2022)
Complications
If skin tears are not properly treated, complications such as pain, delayed healing, infection, cellulitis or sepsis may arise (LeBlanc n.d.).
If a skin tear does not heal within four weeks, it is considered chronic (LeBlanc et al. 2018).
Conclusion
Despite being common among older people, skin tears are preventable and treatable. However, thorough patient assessment and the ability to recognise and categorise skin tears are essential.
Note: This article is intended as a refresher and should not replace best-practice care. Always refer to your facility's policy on preventing and managing skin tears.
Test Your Knowledge
Question 1 of 3
According to the STAR classification system, which category of skin tear is defined by edges that can not be realigned to their normal anatomical position and no skin discolouration?
Topics
References
- Beeckman, D et al. 2020, Best Practice Recommendations for Holistic Strategies to Promote and Maintain Skin Integrity, Wounds International, viewed 16 May 2025, https://woundsinternational.com/best-practice-statements/best-practice-recommendations-holistic-strategies-promote-and-maintain-skin-integrity/
- International Skin Tear Advisory Panel 2020, ISTAP Skin Tear Classification, ISTAP, viewed 16 May 2025, https://www.skintears.org/_files/ugd/9d080f_013dc3fb762541248c24ddbc68581221.pdf
- LeBlanc, K et al. 2018, Best Practice Recommendations for the Prevention and Management of Skin Tears in Aged Skin, Wounds International, viewed 16 May 2025, https://woundsinternational.com/best-practice-statements/istap-best-practice-recommendations-prevention-and-management-skin-tears-aged-skin/
- LeBlanc, K n.d., Skin Tears, WoundSource, viewed 16 May 2025, https://www.woundsource.com/patientcondition/skin-tears
- Victoria Department of Health 2022, Skin Tears: Standardised Care Process, Victorian State Government, viewed 16 May 2025, https://www.health.vic.gov.au/sites/default/files/2022-12/standardise-care-skin-tears.PDF
- Victoria Department of Health 2024a, Identifying and Preventing Skin Problems, Victoria State Government, viewed 16 May 2025, https://www.health.vic.gov.au/older-people-in-hospital/pressure-injuries-and-skin-tears-0/identifying-and-preventing-skin-tears
- Victoria Department of Health 2024b, Classifying and Responding to Pressure Injuries and Skin Tears, Victoria State Government, viewed 16 May 2025, https://www.health.vic.gov.au/older-people-in-hospital/pressure-injuries-and-skin-tears-0/classifying-and-responding-to-pressure-injuries-and-skin-tears
Additional Resources
- International Skin Tear Advisory Panel (ISTAP)
- Resources & Downloadables | ISTAP
- Skin Tears: Standardised Care Process | VIC DoH
- Skin Tear Assessment and Management Guidelines ‘STAR’ Classification (with images) | Mercy Health
- Best Practice Recommendations for Holistic Strategies to Promote and Maintain Skin Integrity | Wounds International
- Best Practice Recommendations for the Prevention and Management of Skin Tears in Aged Skin | Wounds International

