Hyponatraemia, an electrolyte imbalance characterised by low salt concentration in the body, has the potential to cause serious complications, including death (Tee & Dang 2017).
Despite this, syndrome of inappropriate antidiuretic hormone secretion (SIADH), one of the most common causes of hyponatraemia, is often underdiagnosed and undermanaged (Tee & Dang 2017).
What is Syndrome of Inappropriate Antidiuretic Hormone Secretion?
Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is a condition where the body creates excessive amounts of the antidiuretic hormone (ADH) (also called vasopressin) (MedlinePlus 2023).
ADH, which regulates the level of water in the body, is created in the hypothalamus in the brain and secreted by the pituitary gland. It helps the kidneys retain the correct amount of water and is, therefore, responsible for how much water is conserved and eliminated through urination (MedlinePlus 2023; Radhakrishnan & Allarakha 2021).
In someone with SIADH, the secretion of ADH cannot be suppressed. This causes an impaired ability to excrete water through urine output, which disturbs the body’s salt balance and results in the development of hyponatraemia (Sterns et al. 2024).
The resulting hyponatraemia can be acute (developing within 48 hours) or chronic (developing over days or weeks). Acute hyponatraemia is much more dangerous as it develops so rapidly that the brain cells don’t have enough time to adjust properly (MedlinePlus 2023).
In many cases, SIADH is reversible (MedlinePlus 2023).
Causes of SIADH
There are a variety of potential causes for SIADH, including but not limited to:
- Brain and nerve conditions
- Meningitis and encephalitis
- Brain abscess
- Head injury
- Stroke
- Guillain-Barre syndrome
- Hypothalamus or pituitary gland disorders
- Multiple sclerosis
- Shy-Drager syndrome
- Delirium tremens
- Psychosis
- Malignancies
- Small cell lung cancer
- Extrapulmonary small cell carcinoma
- Head and neck cancers
- Olfactory neuroblastomas
- Lung disorders
- Tuberculosis
- Pneumonia
- Asthma
- Cystic fibrosis
- Certain medicines and substances
- Antidepressants
- Anticonvulsants (e.g carbamazepine)
- Antipsychotic agents
- Cytotoxic agents (e.g. cyclophosphamide)
- MDMA (ecstasy)
- Hormone administration
- Vasopressin
- Oxytocin
- Hormone deficiency
- Hypopituitarism
- Hypothyroidism
- Surgery
- Human immunodeficiency virus (HIV) infection
- Genetics.
(Thomas 2023; Sterns et al. 2024; Yasir & Mechanic 2023)
Symptoms of SIADH

Mild SIADH is often asymptomatic, however, the more the body’s salt concentration decreases, the more severe the symptoms become. Patients might experience:
- Nausea and vomiting
- Reduced appetite
- Confusion
- Dizziness
- Hallucinations
- Cognitive disturbances
- Headache
- Muscle weakness
- Muscle cramps
- Impaired gait
- Seizures.
(Yasir & Mechanic 2023; Thomas 2023)
In severe cases, hyponatraemia caused by SIADH can lead to coma, brain herniation, or death (MedlinePlus 2023).
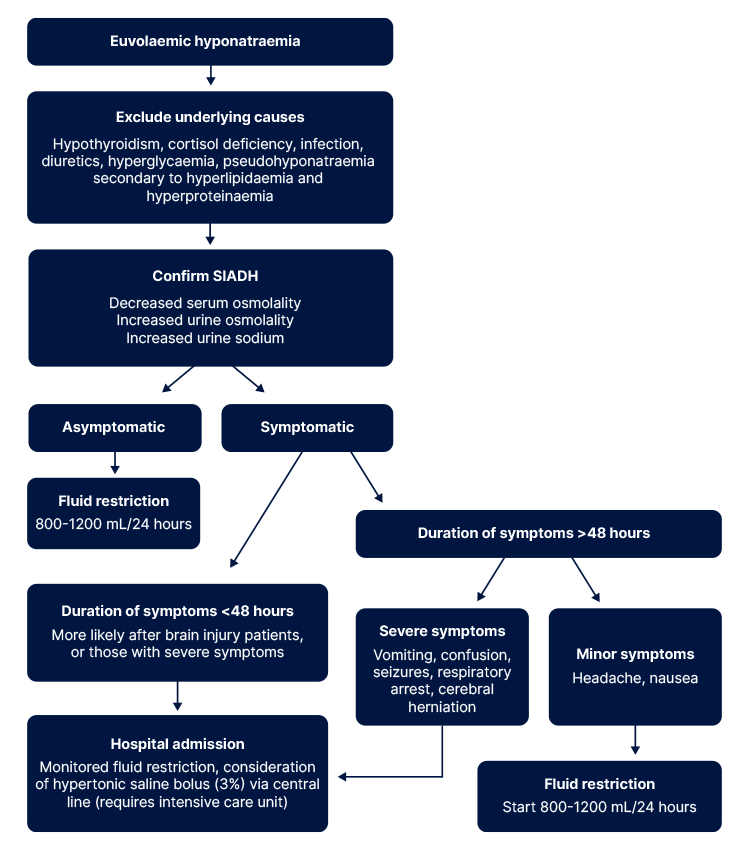
Diagnosis of SIADH
SIADH is diagnosed by taking urine and blood tests to detect the levels of sodium and potassium in the body and measure osmolality (the concentration of these electrolytes in the blood and urine) (CHOP 2018).
The criteria for diagnosis of SIADH is as follows:
- Decreased serum sodium (< 135 mEq/L)
- Decreased serum osmolality (< 275 mOsm/kg)
- Increased urine sodium (> 40 mEq/L)
- Increased urine osmolality (> 100 mOsm/kg)
- Euvolaemia (normal blood fluid volume)
- No other identified cause of hyponatraemia (e.g. diuretic use, hypothyroidism, cortisol deficiency, marked hyperproteinaemia, hyperlipidaemia or hyperglycaemia)
- Correction of hyponatraemia by fluid restriction.
(Yasir & Mechanic 2023; Tee & Dang 2017)
Treatment of SIADH
There are several potential treatments for SIADH, including:
- Addressing underlying causes (e.g. adjusting or changing a medicine that is contributing to the issue)
- High-salt infusion to treat acute cases
- Fluid restriction (limiting the amount of water consumed)
- Medications (e.g. vasopressin receptor antagonists).
(Yasir & Mechanic 2023)
The specific treatment used will depend on:
- The patient’s age, health and medical history
- The extent of the condition
- The patient’s tolerance to medicines, procedures and therapies
- The predicted course of the disease
- The patient’s preferences.
(CHOP 2018)
Management Pathway
Test Your Knowledge
Question 1 of 3
Which one of the following is more dangerous?
Topics
Further your knowledge
 Free
Free
References
- Children’s Hospital of Philadelphia 2018, Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH), CHOP, viewed 18 October 2024, https://www.chop.edu/conditions-diseases/syndrome-inappropriate-antidiuretic-hormone-secretion-siadh
- MedlinePlus 2023, Syndrome of Inappropriate Antidiuretic Hormone Secretion, U.S. Department of Health and Human Services, viewed 17 October 2024, https://medlineplus.gov/ency/article/000314.htm
- Radhakrishnan, R & Allarakha, S 2021, What Causes SIADH?, MedicineNet, viewed 17 October 2024, https://www.medicinenet.com/what_causes_siadh/article.htm
- Sterns, RH, Emmett, M & Forman, JP 2024, Pathophysiology and Etiology of the Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH), UpToDate, viewed 17 October 2024, https://www.uptodate.com/contents/pathophysiology-and-etiology-of-the-syndrome-of-inappropriate-antidiuretic-hormone-secretion-siadh
- Tee, K & Dang, J 2017, ‘The Suspect – SIADH’, Urology, vol. 46, no. 9, viewed 17 October 2024, https://www.racgp.org.au/afp/2017/september/the-suspect-siadh/
- Thomas, CP 2023, Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH), Medscape, viewed 18 October 2024, https://emedicine.medscape.com/article/246650-overview#a5
- Yasir, M & Mechanic, OJ 2023, ‘Syndrome of Inappropriate Antidiuretic Hormone Secretion’, StatPearls, viewed 17 October 2024, https://www.ncbi.nlm.nih.gov/books/NBK507777/