Tonsillectomy is one of the most common surgical procedures undergone by children in Australia (ACSQHC 2021) - but is it being performed more often than necessary?
What are the Tonsils?
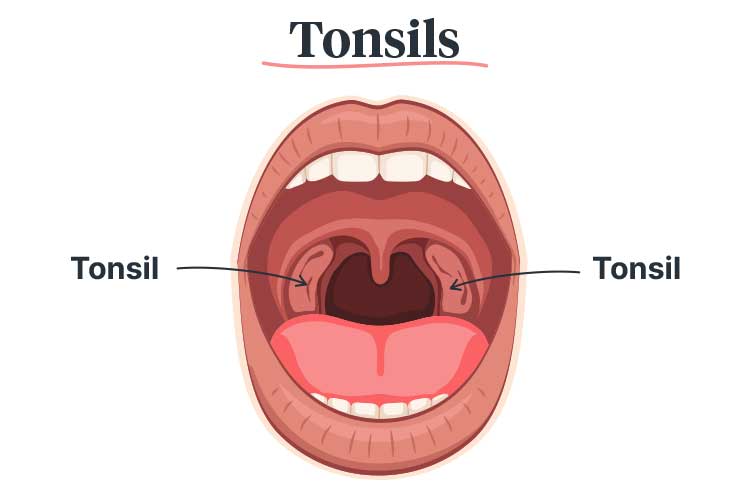
The tonsils, which form part of the immune system, consist of two pads of lymphatic tissue at the back of the throat (one on each side) (Children’s Health Queensland 2023).
More lymph nodes, known as adenoids, sit behind the nose at the back of the throat, out of sight. Together, the tonsils and adenoids help prevent infection by trapping pathogens that enter the nose and mouth and producing antibodies to kill them (Seladi-Schulman 2018).
Despite this, the tonsils and adenoids themselves are prone to infection and inflammation, particularly among children (ACSQHC 2021; Healthdirect 2023a).
Why are Children Prone to Tonsil-related Issues?
Children naturally have large tonsils that grow rapidly between the ages of two and seven. (RCHM 2018).
This is normal - in fact, a person’s tonsils generally reach their full size during childhood (Masters et al. 2023). The adenoids are also at their largest during childhood and may disappear altogether before adolescence (Healthdirect 2023a).
However, while enlarged tonsils and adenoids are common in young children, they can cause respiratory issues if they are large enough to block the airway (Better Health Channel 2021).
Children with large tonsils also tend to breathe through their mouth, which can lead to an increased risk of respiratory tract infections or jaw misalignment (InformedHealth.org 2023).
Common Tonsil-Related Issues Among Children
Tonsillitis

Read: Common Respiratory Tract Infections (RTI)
Tonsillitis is an infection that causes the tonsils to become inflamed and swollen. Tonsillitis is typically caused by a virus, particularly those that cause the common cold, but it can also be bacterial. It can affect anyone, but is most common in children (Healthdirect 2023b; Anderson & Paterek 2023).
Symptoms of tonsillitis may include:
- Sore throat
- Inflamed and painful tonsils, with white patches or pus in some cases
- Fever
- Difficulty or pain when swallowing
- Headache
- Swollen lymph nodes in the neck
- Nausea and vomiting
- Loss of appetite
- Hoarse or muffled voice
- Bad breath
- Stiff neck
- Ear pain
- Abdominal pain
(Healthdirect 2023b; Children's Health Queensland 2023; Mayo Clinic 2022)
Obstructive Sleep Apnoea (OSA)

Read: Obstructive Sleep Apnoea: More Than Just a Bad Night's Sleep
Obstructive sleep apnoea (OSA) is a condition experienced by some children who have large tonsils and adenoids obstructing their airway.
OSA occurs when the upper airway muscles are partially or completely blocked during sleep. A person with OSA will stop breathing, wake up, open their airway and then immediately go back to sleep. This sequence may repeat hundreds of times in one night, impacting the person’s sleep quality (RCHM 2018; Better Health Channel 2021).
While large tonsils and adenoids are the primary cause of OSA in children, other contributing risk factors include obesity, Down syndrome, brain abnormalities and neuromuscular disorders (ACSQHC 2021).
Symptoms of OSA in children include:
- Loud snoring, pauses in breathing or breathing difficulties during sleep
- Choking, gasping or snorting during sleep
- Restlessness and perspiration during sleep
- Unusual sleep positions (e.g. propped up high on pillows)
- Breathing through the mouth instead of the nose during sleep
- Headaches or fatigue in the morning
- Blocked nose, poor appetite or swallowing difficulties
- Concentration difficulties, behavioural issues or learning difficulties due to impaired sleep.
(RCHM 2018)
If left untreated, OSA may cause impaired growth, cognitive and behavioural issues, and even cardiovascular problems (ACSQHC 2021).
What is a Tonsillectomy?
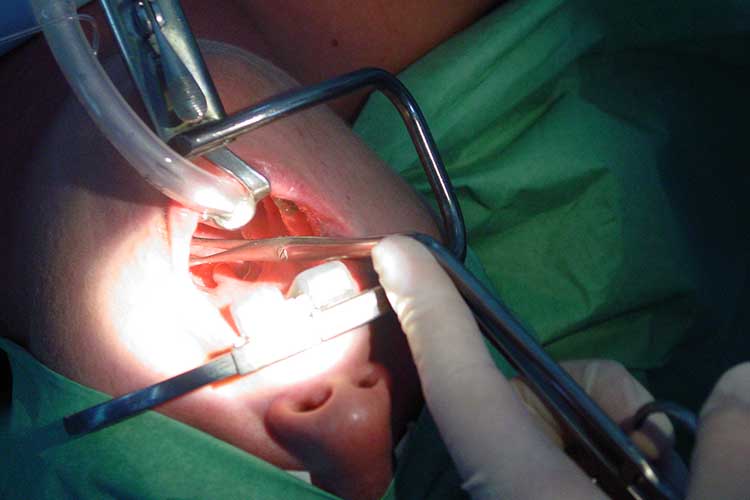
In some cases, children require surgical intervention in order to manage recurrent tonsillitis or OSA (ACSQHC 2021).
This is achieved by performing a tonsillectomy - a procedure wherein the tonsils are surgically removed (Children’s Health Queensland 2023).
Despite the routine use of tonsillectomy in Australia to treat both recurrent tonsillitis and OSA, there is uncertainty surrounding the effectiveness of the procedure (ACSQHC 2021).
Tonsillectomy in Australia
The Fourth Australian Atlas of Healthcare Variation identifies tonsillectomy in children as a key issue, stating that there is an ‘urgent need’ to determine the short and long-term outcomes of the procedure (ACSQHC 2021).
What do we know so far?
Tonsillectomy for Tonsillitis
According to data compiled by the Atlas, tonsillectomy in children who experience recurrent tonsillitis has been found to reduce throat infections, doctor visits and school absences. However, these benefits only appear to last for the first year following surgery.
Furthermore, some children with recurrent tonsillitis recover on their own without the need for surgery (ACSQHC 2021). While there are no Australian guidelines for tonsillectomy in children with recurrent tonsillitis, United States guidelines suggest the procedure be offered to children experiencing:
- Seven or more tonsillitis infections per year, or
- Five or more tonsillitis infections per year for two years, or
- Three or more tonsillitis infections per year for three years.
(ACSQHC 2021)
Tonsillectomy for Obstructive Sleep Apnoea (OSA)
First-line treatment for moderate or severe OSA and enlarged tonsils is generally
Potential Complications of Tonsillectomy
Understanding the possible consequences of a tonsillectomy is important in addition to determining the potential benefits.
Compared to all childhood surgical procedures, tonsillectomy has the highest risk of postoperative complications (ACSQHC 2021). These may include:
- Respiratory compromise
- Pain
- Bleeding
- Dehydration
- Nausea and vomiting
- Speech disorders
- Unplanned hospital readmission
- Death (rarely).
(ACSQHC 2021)
Among these potential complications, the most common is postoperative bleeding, which can be fatal in some cases (ACSQHC 2021).
What Recommendations Have Been Made?
Based on the information compiled by the Atlas, the Australian Commission on Safety and Quality in Health Care recommends that the Australian and New Zealand Society of Paediatric Otorhinolaryngology develop clinical guidelines for tonsillectomy in children. From there, the Commission will develop a clinical care standard with safety and quality indicators (ACSQHC 2021).
Until then, clinicians and parents are left to weigh up the potential risks and benefits of tonsillectomy and make difficult treatment decisions amidst this uncertainty (ACSQHC 2021).
Test Your Knowledge
Question 1 of 3
What is the most common cause of tonsillitis?
Topics
Further your knowledge
 Free
Free Free
FreeReferences
References
- Anderson, J & Paterek, E 2023, ‘Tonsillitis’, StatPearls, viewed 8 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK544342/
- Australian Commission on Safety and Quality in Health Care 2021, The Fourth Australian Atlas Healthcare Variation 2021, Australian Government, viewed 8 May 2025, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/fourth-australian-atlas-healthcare-variation-2021
- Better Health Channel 2021, Sleep Apnoea, Victoria State Government, viewed 8 May 2025, https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/sleep-apnoea
- Children’s Health Queensland 2023, Tonsillectomy, Queensland Government, viewed 8 May 2025, https://www.childrens.health.qld.gov.au/fact-sheet-tonsillectomy/
- Healthdirect 2023a, Adenoids, Australian Government, viewed 8 May 2025, https://www.healthdirect.gov.au/adenoids
- Healthdirect 2023b, Tonsillitis, Australian Government, viewed 8 May 2025, https://www.healthdirect.gov.au/tonsillitis
- InformedHealth.org 2023, Enlarged Tonsils and Adenoids: Overview, Institute for Quality and Efficiency in Health Care, viewed 8 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK536881/
- Masters, KG, Zezoff, D & Lasrado, S 2023, ‘Anatomy, Head and Neck, Tonsils’, StatPearls, viewed 8 May 2025, https://www.ncbi.nlm.nih.gov/books/NBK539792/
- Mayo Clinic 2022, Tonsillitis, Mayo Clinic, viewed 8 May 2025, https://www.mayoclinic.org/diseases-conditions/tonsillitis/symptoms-causes/syc-20378479
- The Royal Children's Hospital Melbourne 2018, Obstructive Sleep Apnoea (OSA), RCHM, viewed 8 May 2025, https://www.rch.org.au/kidsinfo/fact_sheets/Childhood_obstructive_sleep_apnoea_OSA/
- Seladi-Schulman, J 2018, ‘Tonsils and Adenoids Overview’, Healthline, 3 May, viewed 8 May 2025, https://www.healthline.com/health/tonsils-and-adenoids

