Many people have misperceptions about how someone will be affected by stroke.
You might automatically envision mobility difficulties and hemiplegia, or perhaps swallowing problems, or maybe even being unable to speak or communicate.
In reality, there are different types of stroke, and, therefore, different resulting symptoms. It is important to know exactly what type of stroke your patient has experienced in order to predict some of these symptoms.
Stroke, also known as a cerebrovascular accident, is the interruption of blood supply to part of the brain, resulting in acquired (non-traumatic) brain injury (Mayo Clinic 2023a; Brain Injury Association of America 2022).
The disruption of blood flow deprives the affected area of the brain of the nutrients and oxygen it needs to survive, resulting in cell death (Mayo Clinic 2023a).
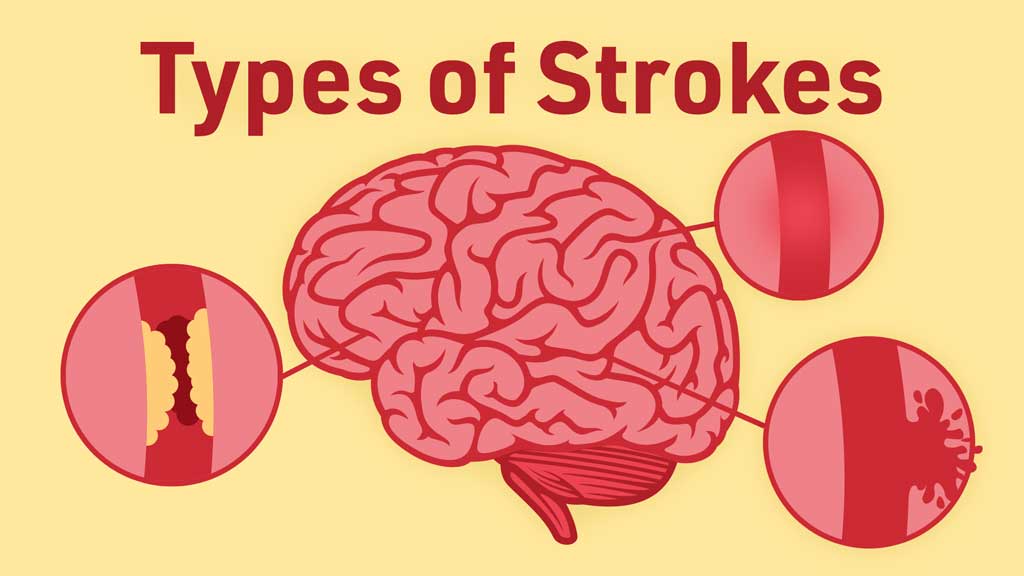
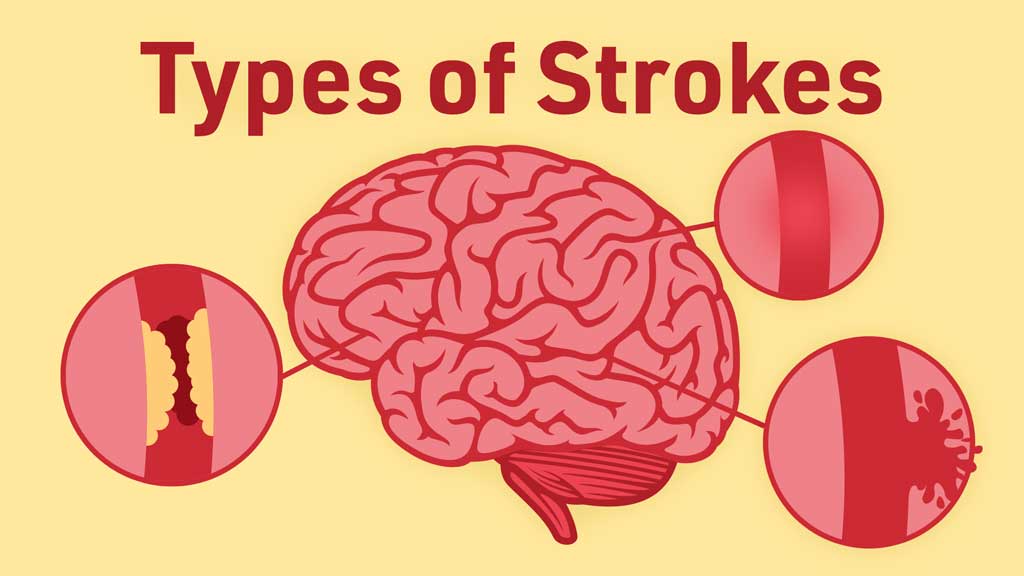
There are two main types of stroke: ischaemic and haemorrhagic.

Ischaemic Stroke
Ischaemic stroke occurs when a thrombus or embolus impairs cerebral blood flow. It is the most common type of stroke, accounting for about 87% of cases (ASA 2019a).
Thrombotic stroke occurs when a thrombus (blood clot) forms and occludes an artery in the brain. This usually occurs in people with atherosclerosis (a build-up of fatty deposits in the arteries), which causes narrowing of the arterial lumen (LeWine 2022).
Embolic stroke occurs when an embolus forms in the circulatory system (usually in the heart or large arteries of the upper chest and neck), dislodges and is carried to the brain, where it occludes a cerebral blood vessel (ASA 2019a).
Haemorrhagic Strokes
Haemorrhagic stroke occurs when there is a rupture in a cerebral blood vessel that causes bleeding in the brain (ASA 2019b).
The main cause of haemorrhagic stroke is hypertension, but it can also be brought on by anatomical defects such as aneurysms, arteriovenous malformations (AVMs) or degenerative changes occurring in arterial walls (Harvard Medical School 2019).
An aneurysm occurs when a weakened area of a blood vessel enlarges and ‘balloons’ out. This section of the blood vessel may continue to weaken until it eventually ruptures and bleeds into the brain (ASA 2018).
It’s estimated that about 5% of people have an aneurysm, but many will not rupture (myDR 2016).
Arteriovenous malformations (AVMs) occur when there is a cluster or tangle of abnormally formed blood vessels. These blood vessels bypass normal brain tissue and divert the blood from the arteries to the veins. If these AVMs rupture they then cause bleeding (Mayo Clinic 2023b).
Symptoms of an AVM will vary depending on its location (Mayo Clinic 2023b).
Manifestations of Stroke
The manifestation of stroke will depend on many factors. When stroke occurs, areas of the brain are deprived of their oxygen supply, causing necrosis of cerebral tissue, and consequently, neurological deficits.
The deficits that may present will depend on the area of the brain involved (Mayo Clinic 2023a).
Left and Right Hemisphere Strokes
When stroke occurs, it’s important to take note of which brain hemisphere it has occurred in, as this will suggest the neurological deficits that have potentially occurred.
Generally, the patient will experience hemiplegia on the opposite side of the area of stroke. For example, if they experiece stroke in the left hemisphere of their brain, they will likely have right-sided weakness or hemiplegia (Yetman 2020).
There are other potential effects that depend on which hemisphere stroke occurred in:
Left hemisphere
- Receptive, expressive or global aphasia (impairment of production and comprehension of language)
- Motor apraxia
- Verbal apraxia.
(Allina Health System 2023)
Right hemisphere
- Spatial and perceptual deficits
- Attention and focusing issues
- Agnosia (difficulty recognising objects, faces, voices or places)
- Anomia (difficulty remembering the names of objects)
- Neglecting the left side of the body
- Difficulty following instructions or answering consecutive questions.
(Allina Health System 2023)
Arterial Ischaemic Strokes
Middle cerebral artery (MCA) stroke

Middle cerebral artery (MCA) stroke occurs when the middle cerebral artery, which supplies the frontal lobe and lateral surface of the temporal and parietal lobes with blood, becomes blocked (Nogles & Galuska 2023).
It’s important to note that individuals who have experienced the same type of stroke will often display different symptoms depending on precisely where and how much of the brain was deprived of oxygen and where cerebral tissue necrosis has occurred.
This is especially important to remember for those who have experienced MCA stroke, as the middle cerebral artery supplies such a vast area of the brain that the deficits are dependent on the areas most damaged.
MCA stroke can have many implications for the individual. These may include:
- Deficits in movement and sensation (contralateral hemiplegia and hemianesthesia)
- Dysphagia
- Impaired speech ability (dysarthria, aphasia)
- Impaired vision and partial blindness (hemianopia)
- Hemineglect
- Incontinence.
(Slater 2023)
Anterior cerebral artery stroke
The anterior cerebral artery supplies blood to most of the anterior section of the interhemispheric cortical surface of the frontal and parietal lobes (Physiopedia 2016).
The deficits left following this type of stroke may include:
- Deficits in movement and sensation (contralateral hemiplegia and hemianesthesia) that are often worse in the lower limbs
- Gait apraxia
- Disinhibition and speech perseveration
- Reduction in speech, motivation or movement (abulia)
- Mental state impairment such as confusion, amnesia, apathy or short attention span.
(Jauch 2022; Das & Saadabadi 2022)
Posterior cerebral artery stroke
Stroke in the posterior cerebral artery will affect the temporal and occipital lobes, impacting the vision of the patient (Kyubu et al. 2020).
Individuals who have experienced this type of stoke will potentially experience blindness in half their vision field (hemianopia) or the inability to perceive colours (Kyubu et al. 2022).
They may also experience dyslexia, memory deficits, aphasia or pupillary dysfunction (Kyubu et al. 2022).
The Future

About one in four stroke survivors will experience another stroke in their lifetime (ASA 2019c).
Therefore, implementing stroke prevention strategies, providing education and decreasing known risk factors for the individual are essential following stroke.
Test Your Knowledge
Question 1 of 3
What is the most common type of stroke?
Topics
References
- Allina Health System 2023, Understanding Stroke, 6th edn, Allina Health, viewed 22 June 2023, https://www.allinahealth.org/health-conditions-and-treatments/health-library/patient-education/understanding-stroke
- American Stroke Association 2019b, Hemorrhagic Stroke (Bleeds), American Heart Association, viewed 22 June 2023, https://www.stroke.org/en/about-stroke/types-of-stroke/hemorrhagic-strokes-bleeds
- American Stroke Association 2019a, Ischemic Stroke (Clots), American Heart Association, viewed 22 June 2023, https://www.stroke.org/en/about-stroke/types-of-stroke/ischemic-stroke-clots
- American Stroke Association 2019c, Prevent a Second Stroke, American Heart Association, viewed 22 June 2023, https://www.stroke.org/en/life-after-stroke/preventing-another-stroke
- American Stroke Association 2018, What You Should Know About Cerebral Aneurysms, American Heart Association, viewed 22 June 2023, https://www.stroke.org/en/about-stroke/types-of-stroke/hemorrhagic-strokes-bleeds/what-you-should-know-about-cerebral-aneurysms
- Brain Injury Association of America 2022, What is the Difference Between an Acquired Brain Injury and a Traumatic Brain Injury?, Brain Injury Association of America, viewed 21 June 2023, https://www.biausa.org/brain-injury/about-brain-injury/nbiic/what-is-the-difference-between-an-acquired-brain-injury-and-a-traumatic-brain-injury
- Das, JM & Saadabadi, A 2022, ‘Abulia’, StatPearls, viewed 22 June 2023, https://www.ncbi.nlm.nih.gov/books/NBK537093/
- Yetman, D 2020, ‘Hemiplegia: Causes and Treatments for Partial Paralysis’, Healthline, 27 January, viewed 22 June 2023, https://www.healthline.com/health/hemiplegia
- Harvard Medical School 2019, ‘Hemorrhagic Stroke’, Harvard Health Publishing, 13 February, viewed 22 June 2023, https://www.health.harvard.edu/a_to_z/hemorrhagic-stroke-a-to-z
- Jauch, EC 2022, Ischemic Stroke Clinical Presentation, Medscape, viewed 22 June 2023, https://emedicine.medscape.com/article/1916852-clinical#b3
- Kyubu, O, Tadi, P & Dossani, RH 2022, ‘Posterior Cerebral Artery Stroke’, StatPearls, viewed 22 June 2023, https://www.ncbi.nlm.nih.gov/books/NBK532296/
- LeWine, HE 2022, ‘Thrombotic Stroke’, Harvard Health Publishing, 22 February, viewed 22 June 2023, https://www.health.harvard.edu/a_to_z/thrombotic-stroke-a-to-z
- Mayo Clinic 2023b, Arteriovenous Malformation, Mayo Clinic, viewed 24 June 2020, https://www.mayoclinic.org/diseases-conditions/arteriovenous-malformation/symptoms-causes/syc-20350544
- Mayo Clinic 2023a, Stroke, Mayo Clinic, viewed 21 June 2023, https://www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113
- myDR 2016, Aneurysm, myDR, viewed 22 June 2023, https://www.mydr.com.au/heart-stroke/aneurysm
- Nogles, TE & Galuska, MA 2023, ‘Middle Cerebral Artery Stroke’, StatPearls, viewed 22 June 2023, https://www.ncbi.nlm.nih.gov/books/NBK556132/
- Physiopedia 2016, Anterior Cerebral Artery, Physiopedia, viewed 22 June 2023, https://www.physio-pedia.com/Anterior_Cerebral_Artery
- Slater, DI 2023, Middle Cerebral Artery Stroke, Medscape, viewed 22 June 2023, https://emedicine.medscape.com/article/323120-overview#a8