Xerosis is a common condition that generally isn’t serious (Cafasso & Sullivan 2023). However, it can significantly affect quality of life, especially if accompanied by itching (Yao et al. 2023).
What is Xerosis?
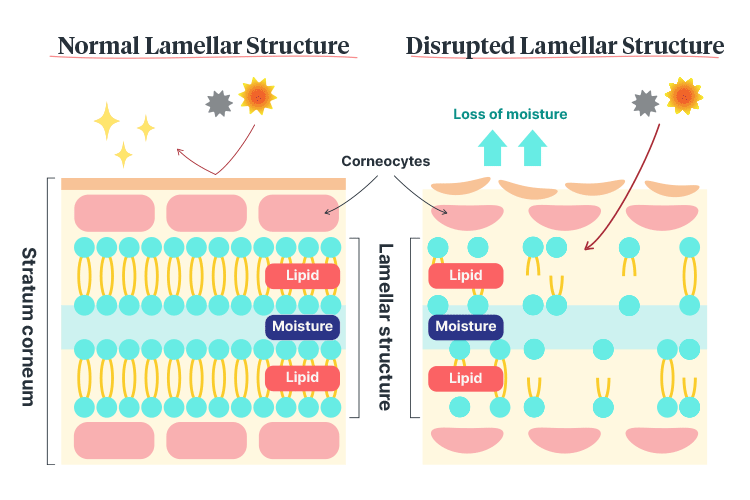
Xerosis (also known as xeroderma or asteatosis) is the medical term used to describe abnormally dry skin, which is caused by dehydration of the stratum corneum (the horny cell layer of the epidermis) (Oakley 2022).
A lack of moisture in the stratum corneum causes the skin surface to lose its flexibility, resulting in splits and cracks. Flaking, scaling, redness or itchiness may also occur (Ciconte 2017).
Skin surfaces affected by xerosis may appear dull, rough or scaly (Oakley 2022). While xerosis can appear anywhere on the body, the most commonly affected areas are the lower legs, arms, scalp and hands (Ciconte 2017).
While the condition is equally common in males and females and affects people of all ages, it is most prevalent in older adults, affecting almost every person over the age of 60 (Oakley 2022).
Why is Xerosis More Common in Older Adults?
Skin is the first part of the body to show age, and changes such as drying, thinning, sagging and wrinkling are inevitable parts of the ageing process (Better Health Channel 2023).
Specific age-related changes in the skin that may contribute to xerosis include:
- Thinning of the epidermis and dermis
- Reduction in strength
- Reduction in the number of cutaneous blood vessels and nerve endings
- Reduction in connective tissue (which includes collagen and elastin)
- Reduction in sweat glands and oil glands
- Reduction in subcutaneous fat
- Decreased moisture-retaining ability
- Decreased thermoregulation
- Reduced ability of the skin to sense the external environment
- Decreased cell turnover
- Decreased skin barrier function
- Decreased immune system response
- Decreased vascularity.
(MedlinePlus 2022; Better Health Channel 2023; Benedetti 2024)
Risk Factors for Xerosis
In addition to older age, risk factors for xerosis include:
Health-related factors
- Genetic factors (e.g. acquired ichthyosis)
- Inflammatory skin conditions (e.g. eczema, psoriasis)
- Certain comorbidities (e.g. thyroid disease, renal disease, diabetes)
- Systemic disease that results in ichthyosis (e.g. lymphoma, malnutrition)
- Certain medicines (e.g. diuretics, cholesterol-lowering drugs, retinoids)
- Infection (e.g. hepatitis B, hepatitis C, HIV)
- Hormonal changes (e.g. menopause, pregnancy)
- Certain psychological conditions (e.g. obsessive-compulsive disorder, anorexia, substance abuse)
- Excessive sweating
- Dehydration
- Weight loss
Environmental factors
- Low-humidity climate
- Cold, dry air
- Direct heat (e.g. central heating, fireplaces)
- Air conditioning
- Chronic sun exposure and damage
- Soaps or detergents with harsh ingredients
- Irritation from rough clothing
Lifestyle factors
- Frequent immersion in water
- Swimming in chlorinated pools
- Long, hot showers or baths
- Excessive handwashing
- Over-cleaning or scrubbing the skin
- Drying skin too vigorously with a towel
(Ciconte 2017; Mayo Clinic 2023; BPAC NZ 2014; Augustin et al. 2019; Cafasso & Sullivan 2023; Oakley 2022)
Symptoms of Xerosis

People with xerosis may experience:
- Skin tightness, particularly after being immersed in water
- Roughness
- Itching
- Flaking, scaling or peeling (can range from mild to severe)
- Fine lines or cracks
- Grey, ashy-looking skin
- Redness
- Bleeding from deep cracks.
(Mayo Clinic 2023)
Potential Complications of Xerosis
- Eczema
- Skin infection (if pathogens enter a break in the skin)
- Overheating
- Food allergies
- Contact allergies.
(Oakley 2022)
How is Xerosis Treated?
Depending on the severity of the dryness, treatment may involve using moisturisers (to add moisture to the skin) and emollients (to soften the skin). Ideally, these should be liberally applied to the affected skin area after washing or when itchy (Oakley 2022).
Generally, the drier the skin, the more thickly an emollient should be applied (especially on the hands) (Oakley 2022).
Moisturisers and emollients help to:
- Decrease itching
- Improve the functioning of the skin barrier
- Prevent irritants and pathogens from entering the affected skin area
- Decrease transepidermal moisture loss
- Attract water to the epidermis from the dermis
- Prevent the escape of moisture from the skin by creating an oily layer (if using in an ointment form)
- Reduce inflammation.
(Oakley 2022; BPAC NZ 2014)
Additionally, patients may require topical steroids or topical calcineurin inhibitors (seek medical direction) (Oakley 2022).
Preventing Xerosis in Older Adults

The following practical strategies may help to prevent xerosis in your patients:
- Identifying and avoiding triggers such as harsh soaps and hot water
- Reducing the frequency and length of bathing
- Using a humidifier in winter
- Using lukewarm water instead of hot water when washing or bathing
- Replacing soaps with gentle substitutes
- Drying the skin by patting it gently rather than rubbing vigorously
- Ensuring adequate nutrition and hydration
- Ensuring fingernails and toenails are trimmed to a suitable length
- Using dressings that are non-adherent and non-adhesive
- Managing incontinence properly
- Reviewing medications (if appropriately qualified to do so)
- Treating skin conditions promptly.
(Oakley 2022; BPAC NZ 2014; VIC DoH 2024; Ciconte 2017)
Test Your Knowledge
Question 1 of 3
One of your clients, Sue, enjoys washing her body with a fragrant soap that she has been using for many years. However, she has recently developed xerosis. What would be the best solution?
Topics
Further your knowledge
 Free
Free Free
Free Free
Free Free
Free Free
Free
References
- Augustin, M, Wilsmann-Theis, D, Körber, A, Kerscher, M, Itschert, M D & Staubach, P 2019, ‘Diagnosis and Treatment of Xerosis Cutis – a Position Paper’, Journal of the German Society of Dermatology, vol. 17, no. 57, viewed 10 February 2025, https://onlinelibrary.wiley.com/doi/10.1111/ddg.13906
- Benedetti, J 2024, Effects of Aging on the Skin, MSD Manual, viewed 10 February 2025, https://www.msdmanuals.com/home/skin-disorders/biology-of-the-skin/effects-of-aging-on-the-skin
- Best Practice Advocacy Centre New Zealand 2014, ‘“Seventh Age itch”: Preventing and Managing Dry Skin in Older People’, Best Practice Journal, no. 63, viewed 10 February 2025, https://bpac.org.nz/bpj/2014/september/dryskin.aspx
- Better Health Channel 2023, Healthy Ageing - The Skin, Victoria State Government, viewed 10 February 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/healthy-ageing-the-skin
- J, Cafasso & D, Sullivan 2023, ‘Xerosis Cutis’, Healthline, 10 April, viewed 10 February 2025, https://www.healthline.com/health/xerosis
- Ciconte, A 2017, Xerosis, Australasian College of Dermatologists, viewed 10 February 2025, https://www.dermcoll.edu.au/atoz/xerosis/
- Mayo Clinic 2023, Dry Skin, Mayo Clinic, viewed 10 February 2025, https://www.mayoclinic.org/diseases-conditions/dry-skin/symptoms-causes/syc-20353885
- MedlinePlus 2022, Aging Changes in Skin, U.S. Department of Health and Human Services, viewed 10 February 2025, https://medlineplus.gov/ency/article/004014.htm
- Oakley, A 2022, Dry Skin, DermNet, viewed 10 February 2025, https://dermnetnz.org/topics/dry-skin/
- Victoria Department of Health 2024, Preventing Skin Problems, Victoria State Government, viewed 10 February 2025, https://www2.health.vic.gov.au/hospitals-and-health-services/patient-care/older-people/skin/skin-preventing
- Yao, D, Gong, X, Ma, Y et al. 2023, ‘The Prevalence and Interventions of Xerosis Cutis Among Older Adults: A Systematic Review and Meta-Analysis’, Geriatric Nursing, vol. 54, viewed 10 February 2025, https://www.sciencedirect.com/science/article/abs/pii/S0197457223002422

